Large
and giant vestibular schwannomas
Clinic of Neurosurgery, Universitary Hospital
Bucharest Romania
Motto:
"If any neurologic surgeon were asked to name
the most difficult tumor to extirpate, his answer
would doubtless
to be the acustic tumor"
Dandy (1)
Abstract
Background: The main objective in treating large and giant
vestibular schwannomas (VS) (large - diameter exceeding
3.5 cm and giant - diameter exceeding 4.5 cm) is their complete removal
without significant morbidity Our experience
on 7 cases (4 females, 3 males, mean age 42.5 years) with marked brainstem compression, operated between 2004-2009 focuses
on factors influencing recurrence and morbidity, especially related to facial nerve
function. These patients were included in a series of 32 consecutive vestibular
schwannoma excisions.
Methods This report is a retrospective analysis of the surgical
outcome of 7 patients with large and giant VS using the retrosigmoid-transmeatal
approach. Several prognostic factors were evaluated: patient age, tumor size
and consistency, extent of surgical removal, concurring hydrocephalus, hearing
loss, facial nerve function, trigeminal nerve
deficits, cranial nerve VI, IX and X palsy,
tongue edema, ataxic gait and motor deficits.
Results: The mean age was 42.3 years, the mean tumor
diameter was 51.8 mm. There were no deaths and the
tumors were histologically benign. Extensive microscopic tumor resection
was performed in 5 cases related to solid tumor's consistency. Preoperatively
hearing loss and high intracranial pressure were encountered in all patients. 4
patients had cerebellar ataxia. Facial anatomical continuity was preserved in 6
cases with solid tumor consistency; 4 patients had a preoperative facial palsy,
a good facial nerve function was achieved in 3 cases - House-Brackmann grade
I/II. We have met other distinctive signs:
cranial nerve V hypoesthesia, VI, IX and X palsy,
tongue edema in 2 cases with slight contralateral motor deficit. All patients
were clinical and MRI monitored at 3, 6 and 12 months postoperatively.
Conclusion: Total resection
associated with a low morbidity rate is possible, avoiding recurrence,
reintervention and severe scar tissue. In cases with subtotal resection,
radiosurgery is recommended to improve outcome.
Key words: large and giant vestibular schwannomas (VS),
surgical approach, facial nerve function
Introduction:
The progress of neurosurgery as a specialty is
related to the history of a vestibular schwannoma (VS) - the more accurate term of the classical acoustic
neuroma, suggesting the tumor origin from the
superior (upper) division of the vestibular nerve, not from the cochlear (also
known as the acoustic) nerve (2).
Microsurgical removal of large and giant VS is
a daunting task to surgeons, presenting a greater challenge in the quest for
total removal - based on a clear surgical strategy, functional cranial nerve
preservation and avoidance of any complications (3-8).
For VS larger than 3 cm, associated
with significant compression of the brainstem, Gamma knife therapy cannot be
used because of the need to
program more than one
isocenter for the radiation dose, exposing normal neural tissue to excess
amounts of radiation (5)(9).
We have made a retrospective
analysis of the surgical outcome of 7 patients with large and giant vestibular schwannomas operated
using the retrosigmoid-transmeatal approach.
Material and methods
From 2004-2009, 32 consecutive VS
resections were performed by the senior author (G.I.) using the retrosigmoid-transmeatal approach. Inclusion criteria were
all VS larger than 3 cm in size, corresponding to grade IV Koos classification.
We have identified in a review of the operations 7 cases with large or
giant VS: 4 females, 3 males, mean age 42.5 years (ranging from 38-68 years)
Preoperative hearing loss - the threshold
retained for useful hearing was 60 decibel - Norstadt classification for
audiometric hearing (10) and high intracranial pressure with obstructive
hydrocephalus were encountered in 2 patients. 4 patients (57.14%) had
cerebellar ataxia; 5 patients (71.42%) had facial numbness, paresthesia; 4 (57.14%)
patients had a preoperative facial palsy; 3 (42.8%) patients had swallowing
difficulties and contralateral motor deficit was observed in 2 (28.57%)
patients
All patients underwent CT, MRI T1 -
weighted imaging before and after Gadolinium (Gd ) administration and T2
- weighted imaging pre and postoperative; measurements were made on the largest
diameter of the tumor excluding intracanalicular components. Tumors classified as large presented a diameter above 3.5
cm, whereas the diameter of giant tumors exceeded 4.5 cm. There were 4 (57.14%)
cases with giant tumors and 3 (42.85%) cases with large tumors (mean
tumor diameter was 51.8 mm). The tumor's consistency was classified as solid or
cystic using T1 and T2 - weighted image with Gd
administration. We found that 28.5% of VS (2 cases) included in our study
contained cystic elements.
Surgery was performed using the
retrosigmoid - transmeatal approach in the lateral decubitus. In 2 cases a
temporary shunt was placed intraoperatively to relieve hydrocephalus. A
retrosigmoid suboccipital craniotomy of 4 cm diameter was made to expose the
posterior part of the sigmoid sinus and the inferior part of the transverse
sinus. We favor such an approach for the following arguments: a wider field of
action, direct visualization of anterior inferior cerebellar artery (AICA) and
other brain stem vessels, dissection of all surfaces of the acoustic tumor
always under direct vision, identification of the facial nerve in the lateral
angle of the internal auditory canal, ready access to the facial nerve when
either anastomosis or graft reconstruction may be necessary.
The surgical technique was based on
internal tumor debulking made in a systematic fashion. The ultimate goal of VS surgery being
cranial nerves preservation, tumor removal is merely a byproduct. The surgical
steps after dural opening tangent to sinuses are:
-cisterna magna opening to allow cerebellar
retraction, made by applying a single broad malleable blade from below upwards
-identification of the double arachnoid membrane
protecting the cerebellum, lower cranial nerves, anterior inferior cerebellar
artery (AICA)
-the tumor capsule is separated from the cerebellum
and the inferior tumor part is elevated from the lower cranial nerves and brain
stem
-centrifugal, rapid, tumor debulking, to shrink tumor
using tumor forceps, dissector (CUSA may perforate the arachnoid layer and
damage the neural vasculature!); it's better to leave a shelf of tumor
"capsule" all around to avoid injury to all structures outside it
-the tumor is further separated at the upper pole from
the trigeminal nerve and pons
-the meatus acusticus internum is exposed in two
stages: drilling away the back wall, carrying out the remaining upper tumor; optional
drilling the fundus. It is mandatory to avoid the semicircular canals (laterally)
and the jugular bulb (inferiorly) whilst drilling; copious water irrigation
whilst canal drilling to prevent thermal injury to VII & VIII complex;
stripping the dura from canal; waxing bone edges to keep the field bloodless;
placement of muscle patch in IAC after tumor removal to prevent CSF leak
-fine dissection close to nerves - the remainder is
separated from the facial nerve, brain stem, abducens nerve using a water-jet
dissection. In our series, the facial nerve was displaced over the medial
aspect of the tumor. Dissection
was made bidirectional from the medial and lateral
direction meeting near the meatus acousticus internum where most adherences are
to be seen. A small part of the capsule attached to the nerve should be
leaved. Several blood vessels should be preserved:
internal auditory artery, AICA and its branches - the most displaced vessel,
SCA, brain stem perforators; also the petrosal and mesencephalic veins.
-dura is closed watertight using a wet fibrinoid-based
collagen fleece (Tachocomb), bone flap is refixed.
-for extensive adherences of the tumor to the facial
nerve and also to the brainstem in 2 (28.57%) cases a partial tumor removal was
performed; no bipolar coagulation was used for hemostasis in this situation:
applying a cottonoid, a Gelfoam or Surgicel is temporarily sufficient. Trauma
to arachnoidless brain stem surface can be predicted on pre-op CT/MRI. Possible
postoperative complications could be induced by: forceful retraction of a
densely adherent tumor, traction on the bridging vessels wich may lead to intra-pontine
hemorrhage and coagulation of perforators that can induce brain stem
infarction. To avoid such complications, tumor feeders should be coagulated and
sectioned where they enter the tumor; also staying within the tumor arachnoid
holds the key.
Functional outcome was measured
using the Karnofsky scale at 3, 6,
12 months postoperatively. Several prognostic
factors were evaluated: patient age, tumor size and consistency, extent of
surgical removal, concurrent hydrocephalus, hearing loss, facial nerve function
according to House-Brackmann scale, trigeminal nerve
deficits, cranial nerve VI, IX and X palsy,
tongue edema, ataxic gait, motor deficits.
Results
Extensive microscopic tumor resection was
performed in 5 (71.42%) cases; diagnosis was confirmed by histopathology in all
cases. There were no deaths and the tumors were histological
benign (Fig.1). Partial tumor removal was performed for 2 cystic tumors
were the arachnoidal plane was poorly defined, with
severe adherences to brainstem and facial nerve, extensive bleeding and
cerebellar edema.
A B C
D E F G
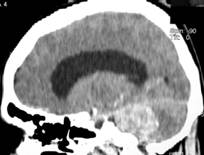
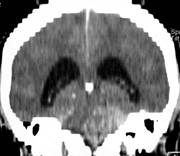
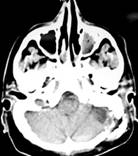
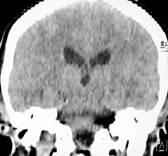
Fig. 1 Preoperative cerebral CT
showing giant VS (51 mm) with obstructive hydrocephalus (A-C); postoperative
cerebral CT after 1 year follow-up showing complete resection (D, E); another
case with giant VS (57 mm) showing pre and postoperative CT
Facial nerve anatomical continuity was
preserved in 6 (85.71%) cases with solid tumor consistency and a good facial
function was achieved in 3 (42.85%) cases - House Brackmann grade I/II. For 4
(57.14%) patients with giant VS, the facial nerve deficit worsened
postoperatively with respect to House-Brackmann grading scale by III grades, the face was rehabilitated with plastic surgery techniques.
We have noticed a rapid tumor
growth, short symptom duration and facial nerve involvement in 2 cystic tumors
were a partial resection was performed.
The Karnofski score at discharge
was superior to 80%. The major complications in this series were: 3 (42.85%)
patients with cranial nerve V hypoesthesia, 5 (71.42%) patients with increased facial numbness, 4 (57.14%) patients with transient VI, IX and X palsy, tongue edema and
2 (28.57%) cases with contralateral motor deficit. These
patients recovered well within 6 months after operation.
In 2 cases with partially resected cystic
tumors, at 12 months after the operation we have noticed on CT and MRI the same
dimensions of the tumor remnants.
Discussion
VS are typically slow growing,
benign skull base tumor of cerebellopontine angle, with natural unpredictable
evolution and annual growth rate between 0.2-2 mm; they originate from the
intracanalicular part of the vestibular nerve, in the region of the transition
zone between central and peripheral myelin (2).
While VS was first described by Eduard
Sandifort in 1777, the first successful surgical removal was achieved by Sir Charles
Balance in 1894, cited by (2). Several neurosurgical pioneers made major
advancements in managing this usually benign skull base tumor: F. Krause who
introduced the retrosigmoid approach to the cerebellopontine angle and H.
Cushing who advocated for subtotal removal and was the first to reduce
mortality from 50 to 7.7% - cited by (11). W. Dandy (1) recommended total
excision with meticulous capsule dissection as goal of surgery in order to
prevent recurrences, with an acceptable low mortality of 2.4%. In 1967 Olivecrona
(12) proposed to preserve the facial nerve, achieving this in 20% of his 304
patients with a total tumor removal in 217 patients and a mortality rate rising
up to 23%.
The translabyrinthine approach was adopted by
Panse in 1904 - cited by (2) as a method to achieve tumor removal preserving
the facial nerve. In 1964 House (13) introduced operating microscope for
translabyrinthine approach and in 1965 Rand and Kurze - cited by (2) were the
first to introduce an operating microscope for the transmeatal posterior fossa
approach.
Yasargil (14) improved the microsurgical
technique, emphasizing the importance of the brain stem arterial supply and the
need to optimize the preservation of facial nerve function. These technical
advances have led to a 50% reduction in mortality, a rate of complete tumor
removal reaching 85% and to a successful anatomical preservation of the facial
nerve in 80% of the cases.
The management of VS has evolved
significantly with the advent of new radiological diagnostic procedures (high
resolution CT, multiplanar MRI) that allow early diagnosis of small and medium
size VS; safe, modern anesthesia, development and refinements in the
microsurgical techniques, neurophysiological intraoperative monitoring and working
in multidisiplinary teams have led to a dramatic improvement in clinical
outcome, with an operative mortality of around 1% and a rate of total tumor
removal close to 95% (2-9)(15-24).
In some expert hands: Koos W. (18),
Rhoton Al. (21), Samii M. (2)(6), Noren G., Regis J., Pellet W., Cannoni M. -
cited by (11), the preservation of useful hearing (Gardner-Robertson 1 or 2)
has been achieved in selected small lesions with very good preoperative hearing
and also the possibility of preserving normal facial motor function in many cases
(House-Brackman 1 or 2).
Although surgical procedures could
be complex and difficult, even in
large and giant VS compressing the brainstem, a complete tumor removal has become the rule in many
cases, preserving all cranial nerves in exceeding
numbers, without additional morbidity or
mortality. In many cases the VIIth nerve may be so thin that it
could be be confused with the arachnoid when very severely compressed. There
are various anatomical relationships encountered during resection; nerve
stimulator, electrophysiology may
allow a gentle separation of VII nerve from tumor by using micro dissector
& sharp arachnoid dissection (6)(7)(18).
Brainstem compression, even
brainstem dislocation, cerebellum and severe fourth ventricle compression can
produce ventricular dilatation; the VII & VIII complex, lower cranial nerves
severely stretched occur in large or giant VS (10)(18).
The most common clinical signs (5)
are: cophosis, cerebellar ataxia, symptoms of raised intracranial pressure
(headache, papilledema) and symptoms of normal pressure hydrocephalus in elderly
(gait disturbance, dementia and incontinence). In our series a temporary shunt
was placed intraoperatively to relieve hydrocephalus in 2 cases; generally the need
of a preoperative shunt was as high as 66% in ancient series (14), others
consider shunting rarely required because total surgical excision is sufficient
(7).
The approach is controversial: many
surgeons prefer the retrosigmoid approach in the sitting, semi-sitting or
lateral position (2-8)(15)(17-19)(21)(23). However Sami (6) reported a high
incidence of hematoma after retrosigmoid removal of cystic tumors in the
semisitting position, as well as air embolism irrespective of anesthetic
monitoring measures taken to prevent this complication. In the lateral position
the peritumoral veins may generate intraoperative bleeding (5). The
translabyrinthine approach is advocated by ENT surgeons for good tumor exposure
with minimal retraction of the cerebellum, early facial nerve identification
and eases the repair of the facial nerve when it is transected (5)(13)(15)(16)(20)(24)(25).
The disadvantages of the translabyrinthine approach (4) are: longer operating
times, higher rates of postoperative facial paralysis and the risk of
cerebrospinal fluid leak.
In large VS, Anderson (3) described a combined
translabyrinthine-retrosigmoid approach especially for more lateral giant
tumors that extend to the fundus of the IAC. The rates of preserving good facial
nerve function are similar among the retrosigmoid, translabyrinthine and middle
fossa approaches in large VS: 42-52.6% with early identification of the root
entry/exit zone and caution in tumor excision in the extrameatal region just
outside the porus acusticus (5). Only 18% of operated patients have excellent
facial nerve function (House-Brackmann grade I/II) explained by the bad initial
clinical status, the tumor size and the lack of systematic intraoperative
facial monitoring (5)(8)(17)(19)(23). According to Sami (6) facial nerve anatomical results (of 200
cases of grade T4 VS, total removal was achieved in 98% and anatomical facial
nerve preservation was possible in 98,5%) were not correlated with functional
results, while size was well correlated with facial function. Even when the
facial nerve is left anatomically intact, surgical interventions can have
esthetic and functional consequences which greatly reduce the quality of life (4).
Removal of large and giant residual
or recurrent VS is more difficult due to scar tissue and the absence of a clear
arachnoid plane between tumor and brainstem, vessels, and nerves even for the
most experienced surgeon (11,18). When excision is incomplete, the recurrence
rate is usually high, depending of VS cellularity and vascularisation (7).
Recurrence rate reported was of 0-3.9% for gross total removal; 9.4-29% for
near total resection as a result of surgical devascularization and 25-65% for
subtotal resection, especially in the midcerebellopontine angle after the
translabyrinthine approach (24). Vestibular schwannomas can relapse 10-15 years
postoperatively (10% of patients) even when surgeons have the impression that
these have been completely removed (4). The growth rate of residual or
recurrent VS is unpredictable: most authors reported a very low recurrence rate
after complete tumor excision; however, a higher recurrence rate after subtotal
removal has also been observed in 44-53% of patients (5). In cystic tumors (26)
a rapid tumor growth with possible vascular compression led to a less
favourable outcome than solid tumor, also some tumor remnants may not grow.
Also cystic VS demand careful dissection and may be subtotally resected for
various reasons: the arachnoid plane is not easily preserved as it is densely
adherent to the surrounding structures; the cranial nerves are displaced in a
relatively uncertain position; cyst formation may predict a more intimate
involvement of the neural tissue; high tendency to postoperative bleeding;
dissection of the facial nerve from the tumor is more difficult (5)(6)(22).
For subtotal tumor debulking
confirmed by MRI at 3 months, 6 months to 1 year postoperatively, the
alternatives are (5)(6)(9)(17)(22)(26):
-planned staged approaches - first tumor debulking via
a retrosigmoid approach followed by a second stage translabyrinthine resection
of the residual tumour
-wait and see - in case a a small and stable residual
tumor in elderly patients
-subtotal tumor debulking followed by stereotactic
radiotherapy which can offer excellent facial nerve function in 85.7% patients
with House-Brackmann grade I/II (1)
and tumor growth control. At the time of radiosurgery the tumor size is
diminuished < 20 mm and radiosurgery could be made with a peripheral dose
11-13 Gy and in the tumor centre the dose should be 22-26 Gy.
Conclusion
VS is a benign tumor in a malignant
location (2). Progressive improvement in the results of VS surgery was possible
owing to: better clinical preoperative deficits evaluation, tumor size (the
smaller the tumor, the better the outcome !), imaging innovations, intensive
care, intraoperative monitoring, advent of microsurgery and of course
increasing surgical experience (6-8)(18).
Complete VS removal at one stage
while preserving neurological functions and the quality of life should be the
optimal treatment, thus avoiding recurrency, reintervention and severe scar
tissue.
For large and giant VS the optimal
treatment should be tried; however an alternative could be the combined staged
therapy: subtotal intracapsular
resection relieving mass effect and brainstem compression at the first stage,
follow-up and stereotactic radiosurgery at a second stage for the residual
tumor.
References:
Dandy
W.E. - Results of removal of acustic tumors by the unilateral approach, A.M.A.
Arch. Surg. 1941, 42: 1026-1043
Samii
M. - Vestibular schwannomas, Sindou M. - Practical Handbook of Neurosurgery,
Springer Wien New York, 2009, 333-345
Anderson
D.E., Leonetti J., Wind J.J. et al. - Resection of large vestibular
schwannomas: facial nerve preservation in the context of surgical approach and
patient assessed outcome, J.Neurosurg. 2005, 102 (4): 643-649
Fuentes
S., Arkha Y., et al. - Management of Large Vestibular Schwannomas by Combined
Surgical Resection and Gamma Knife Radiosurgery, in Regis J., Roche P.H. -
Modern Management of Acustic Neuroma, Karger 2008, 79-82
Laghmari
M., Ouahabi A. El., Derraz S., Khamlichi A. El. - Treatment of large vestibular
schwannomas: Towards a compromise between recurrence and facial function
preservation, Pan Arab Journal of Neurosurgery, 2009, vol.13, 1: 31-39
Samii
M., Gerganov V., Samii A. - Improved
preservation of hearing and facial nerve function in vestibular
schwannoma surgery via the retrosigmoid approach in a series of 200 patients,
J. Neurosurg 2006, 105: 527-535
Turel
K.E. - Surgical techniques & pitfalls in acustic neuroma, Romanian
Neurosurgical Congress, Timisoara 2003.
Yamakami
I., Uchino Y.,Kobayashi E. et al. - Removal of large acoustic neurinomas
(vestibular schwannomas) by the retrosigmoid approach with no mortality and
minimal morbidity, J. Neurol Neurosurg
Psych 2004, 75: 453-458
Lunsford
L.D, Niranjan A., Flickinger J.C., Maitz A., Kondziolka D. - Radiosurgery of
vestibular schwannomas: summary of
experience in 829 cases, J. Neurosurg. 2005, 102 (Suppl): 195-199
Malis
Li - Nuances in acoustic neuroma surgery, Neurosurg. 2001, 49: 337-341
Regis
J. et al. - Introduction, in Regis J., Roche P.H. - Modern Management of
Acustic Neuroma, Karger 2008, 1-5
Olivecrona
H. - Acustic tumors, J. Neurosurg 1967, 26: 6-13
House
W.F. - Translabyrinthine approach, in House W.F., Luetje C.M. (eds) - Acustic
Tumors, Baltimore, University Park Press 1979, 43-87
Yasargil
M.G. et al. - Microsurgical approach to acoustic neuromas, Adv. Tech. Stand.
Neurosurg. 1977, 4, 93-129
Briggs R.J., Fabinyi G., Kaye A.H. - Current
management of acustic neuromas: review of surgical approaches and outcomes,
J.Clin Neurosci 2000, 7: 521-526
Day
J.D., Chen D.A., Arriaga M. - Translabyrinthine approach for acoustic neuroma,
Neurosurgery 2004, 54: 391-395
Iwai
Y., Yamanaka K., Ishiguro T. - Surgery combined with radiosurgery of large
acoustic neuromas, Surg. Neurol 2003, 59: 283-289; discussion: 289-291.
Koos
W.T., Matula C., Lang J. - Color Atlas of Microneurosurgery of Acustic
Neurinomas, Thieme, 2002, 184-190.
Jung
S., Kang S.S., Kim T.S. et al. - Current surgical results of retrosigmoid
approach in extralarge vestibular schwannomas, Surg. Neurol 2000, 53: 370-377;
discussion 377-378
Mamikoglu
B., Wiet R.J., Esquivel C.R. - Translabyrinthine approach for the management of
large and giant vestibular schwannomas, Otol Neurotol 2002, 23: 224-227
Rhoton
A.L. Jr. - The cerebellopontine angle and posterior fossa cranial nerves by the
retrosigmoid approach, Neurosurgery 2000, 47: S93-S129
Ricardo
R., Neto M.C. et al. - Treatment of large and giant residual and recurrent
vestibular schwannomas, Skull Base 2007, 17(2): 109-117.
Seol
H.J., Kim C.H.,Park CK et al. - Optimal extent of resection in vestibular
schwannoma surgery: Relationship to recurrence and facial nerve preservation,
Neurol Med Chir (Tokyo) 2006, 46: 176-180; discussion 180-181
Sluyter
S., Graamans K,Tulleken C.A. et al. - Analysis of the results obtained in 120
patients with large acoustic neuromas results obtained in 120 patients with
large acoustic neuromas surgically treated via the
translabyrinthine-transtentorial approach, J. Neurosurg 2001, 94: 61-66
Brackmann
D.E., Cullen R.D., Fischer L.M. - Facial nerve function after translabyrinthine
vestibular schwannoma surgery. Am Otolaryngol Head Neck Surg 2007, 136: 773-777
Wandong
S., Meng L., Xiangang L. et al. - Cystic acoustic neuroma, J.Clin Neurosci
2005, 12: 253-255