INTRODUCTION
Fractures of the
shaft of the femur are a major cause of morbidity and mortality in patients
with lower extremity injuries. With the exception of infractions through
pathologic bone, violent forces are needed to create these fractures. Fractures
of the shaft of the femur can be life-threatening from an open wound, fat
embolism, adult respiratory distress syndrome, or resultant multiple organ
failure.
Even
with survival of the initial trauma, many patients suffer major physical
impairment as a result of these fractures. Functional loss does not arise from
any inherent problem with fracture healing. This longest and strongest of the
human bones possesses a well-vascularized, thick envelope of muscles that
predictably promotes rapid fracture healing in most patients. Rather,
disability usually results from fracture shortening, fracture malalignment, or
prolonged immobilization of the extremity by traction or casting in an attempt
to maintain fracture length and alignment during the early phases of healing.
Even minor degrees of shortening and malalignment can eventuate in a limp and
posttraumatic arthritis. Therefore, the art of femoral fracture care is a
constant balancing of the often conflicting goals of anatomic alignment and
early functional rehabilitation of the limb.
The
history of femoral fracture management reflects this underlying dilemma. Before
the turn of the century, most treatments involved splinting or encasing the
thigh with a variety of materials. The early use in ancient civilizations of
wood splints wrapped with sinews of leather or fibrous plants110 and various
fabrics encased with wax2 gave way to bandages stiffened with gum324 and, more
recently, fabrics hardened with plaster of Paris.212 None of these materials
alone, however, offered sufficient strength to maintain fracture alignment. The
advent of skeletal radiography at the end of the 19th century clearly
demonstrated the mechanical inadequacies of these traditional treatments.
In
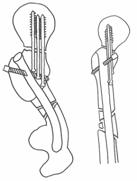
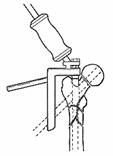
1907, Steinmann334 introduced his first traction pin apparatus, and in 1909,
Kirschner213 proposed his alternative traction design featuring a
small-diameter wire placed under tension (Fig. 27-1). The application of the
Thomas splint, which provides countertraction on the leg through its ring, allowed
for improved control of the traction forces. Modifications in the Thomas splint
since its first clinical use during World War I for the transport of casualties
with femoral fractures have enhanced the mobility of both the patient and the
joints of the injured leg. The basic traction techniques, however, have
remained unchanged for nearly a century.
Early
attempts at internal fixation of femoral fractures were fraught with serious
complications, especially infection and implant failure. The concept of
intramedullary fixation was applied early to fractures of the femoral shaft.
Although isolated cases of intramedullary nailing were reported early in the
century, the modern era of nailing was ushered in by Küntscher.182 His 1939
presentation to the Medical Society of Kiel of his first case of intramedullary
fixation using a V-shaped cross-section-designed nail was followed 4 months
later by his report of 12 additional cases to the German Surgical Society in
Berlin. The initial response to his work was unfavorable. Many of his
colleagues condemned the concept as 'nonphysiologic' and predicted a
disastrously high nonunion rate. The excellent clinical results, however,
resulted in the wide dissemination of the technique in Europe during World War II
and in North America after the war.
The
Küntscher technique for femoral nailing has been refined and embellished over
the last 50 years. Changes have included alterations in both the
cross-sectional and longitudinal design of the nail, modifications in the
technique of its insertion, the use of fluoroscopy for closed nailing, and
innovations in instrumentation. Recent improvements in the mechanical
properties and design of intramedullary nails have stimulated their use in
increasingly more complex fractures.
SURGICAL ANATOMY
The femoral
shaft is essentially a tubular structure. It flares posteriorly along the linea
aspera, where its cortical thickness is the greatest. The linea aspera (Latin
for rough line) serves as a site of attachment for the fascia. The proximal and
distal metaphyseal widening of the tube in the subtrochanteric and
supracondylar regions of the bone results in stress concentration at these
levels. Pathologic fractures, especially in the elderly, commonly occur at
these metaphyseal-diaphyseal junctions. The most prominent feature of the
femoral shaft is its anterior bow or antecurvature. Wide individual variations
exist in the magnitude of this bow. The normal physiologic bow often is
increased in certain pathologic conditions, such as fibrous dysplasia and Paget
disease. The clinical importance of the antecurvature of the shaft has long
been appreciated. Most modern intramedullary nails are prebent, with an average
10- to 12-mm-high arch at their midpoints to accommodate the bow. Straight, stiff
implants used in the early years of femoral nailing straightened the shaft,
leaving a posterior gap at the fracture site. Straight nails also resulted in
fracture comminution and occasionally even perforation of the anterior cortex.
The
femoral shaft is subjected to major musculature forces that deform the thigh
after a fracture (Fig. 27-2). The action of the gluteal musculature that
inserts on the greater trochanter abducts the proximal femur after
subtrochanteric and high proximal shaft fractures. These proximal-third
fractures of the shaft also are flexed and externally rotated by the action of
the iliopsoas muscle's pull on the lesser trochanter. The adductor muscles span
most shaft fractures and exert a strong axial and varus load to the bone. Distal
shaft fractures, especially those extending into the supracondylar region, tend
to angle into flexion through the pull of the gastrocnemius muscle. Adjustments
in traction or bracing devices are needed to counteract these deformity
muscular forces.

Fig.27-2
Fortele musculare deformatoare de pe femur: A.abductori; B.iliopsoas;
C.adductori; D.originea gastrocnemian.Fortelor de angulare mediale li se
opun fascia lata (E). Potentiale zone de leziune vasculare sunt hiatul
adductorilor si perforantele din artera femurala profunda.
The
quadriceps musculature and hamstring musculature function within well-defined
compartments (Fig. 27-3). The thigh contains three distinct fascial
compartments. The anterior compartment encases the quadriceps femoris,
sartorius, iliacus, psoas, and pectineus muscles, as well as the femoral artery
and vein, femoral nerve, and lateral femoral cutaneous nerve. The medial
compartment contains the gracilis, adductor longus, adductor brevis, adductor
magnus, and obturator externus muscles, along with the profundus femoris
artery, obturator artery and vein, and obturator nerve. The posterior
compartment includes the biceps femoris, semitendinosus, semimembranosus, and a
portion of the adductor magnus muscles, as well as branches of the profundus
femoris artery, sciatic nerve, and posterior femoral cutaneous nerve. The thick
lateral intermuscular septum divides the anterior and posterior compartments.
The medial and posterior intermuscular septa are much thinner. Because of the
high volume of these three compartments, compartmental syndrome of the thigh is
much less common than that of the leg. Severe bleeding into one or more
compartments is necessary to elevate the compartment pressure above the
critical level.342 The distinction between the normal swelling after a shaft
fracture and an early thigh compartmental syndrome often requires the
measurement of intracompartmental pressures.
The
femur possesses a rich vascular supply. The arterial supply is derived mainly
from the profundus femoris artery. Although some anatomic variations occur in
humans, the nutrient vessel usually enters the bone proximally and posteriorly
along the linea aspera. In his cadaver dissections of adult femora, Laing184
found that there was usually only a single nutrient vessel, and in none of his
specimens did a major artery enter the lower third of the shaft. The maximum
number of nutrient vessels that he noted in any femur was two. After
penetrating the posterior cortex, the nutrient vessel arborizes proximally and
distally to provide the endosteal circulation to the shaft.
Fig.
27-3 Sectiune transversala coapsa cu evidentierea celor
trei compartimente
Most
of the periosteal vessels also enter the bone along the linea aspera. They
align themselves perpendicularly to the cortical surface with few, if any,
traversing along the periosteum longitudinally. Because of this perpendicular
orientation of the periosteal vessels, they seldom are extensively stripped
during fractures except during severe open injuries. Preservation of this
periosteal circulation is a high priority during any open surgical procedure on
the femur. Damage to the vessels is minimized by avoiding any soft-tissue
stripping of the linea aspera. Although broad bands or tapes around the shaft
should be shunned, simple cerclage wires alone will not devascularize the
cortex because there is little or no longitudinal flow in the periosteal
vasculature. Severe traumatic or operative damage to the periosteal vessels
will result in delayed fracture healing.
The
microcirculation of the femur is similar to that of the diaphyses of other long
bones. Although their contribution is controversial, endosteal vessels are
thought to provide (under normal physiologic conditions) circulation to the
inner two thirds to three quarters of the cortex.281,282,283 They anastomose
with the scattered blood vessels of the periosteal circulation. The normal
blood flow is centrifugal, although some blood returns to the large venous
sinusoids of the medullary canal. The periosteal arteries normally provide flow
limited to the outer one quarter of the cortex, especially posteriorly along
the linea aspera at the site of their penetration into the bone.
After
diaphyseal fractures, the circulatory pattern is radically altered. In the rare
nondisplaced fracture of the shaft, the endosteal supply can be relatively
undisturbed and remain dominant. With most fractures, however, the major
fragments displace, resulting in complete disruption of the medullary vessels.
Proliferation of the periosteal vessels is the paramount vascular response to
the fracture. The rapidly enhanced periosteal circulation is the primary source
of cells and growth factors for healing. The medullary supply eventually is
restored later in the healing process. Once reconstituted, the medullary
circulation again gains dominance.
The
effect of intramedullary nails on the diaphyseal circulation has been studied
extensively by Rhinelander and colleagues.283 Intramedullary nails have the
theoretic disadvantage of preventing restoration of the normal endosteal flow
during fracture healing. Cylindrical or tubular nails that completely fill the
canal can have a deleterious effect on reconstitution of the medullary arterial
and venous flow. The impedance of venous outflow may have as profound an effect
on blood flow to the fracture as any damage to the arteries. Fortunately, no
commercially available nails possess such a circular cross-sectional design.
Cloverleaf, diamond-shaped, fluted, flanged, delta, and other nails provide
potential space for neovascularization of the endosteum. Restoration of endosteal
vessels occurs quickly after fracture when such nails are used. During the
early stages of fracture healing, the periosteal circulation appears to be able
to maintain vascularity to the outer half of the cortex, even with complete
filling of the canal with an intramedullary nail.283 The rapid healing and
remodeling of fractures after closed intramedullary nailing attest to the
abundant collateral circulation to the femoral shaft.
Nearly
all open procedures on the femoral shaft should be performed through a
longitudinal lateral incision. For rare specific indications, the distal
metaphyseal-diaphyseal junction can be approached medially by elevation of the
vastus medialis obliquus muscle. The anterolateral approach to the shaft
through the substance of the vastus intermedius muscle should be avoided.
Postoperative adhesions between the individual muscles of the quadriceps
resulting in knee contractures are common with this latter approach.
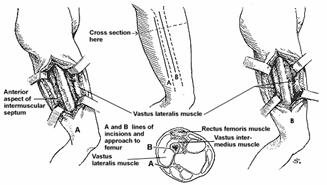
The
lateral approach uses an incision of variable length over the lateral aspect of
the thigh along a line from the greater trochanter to the lateral femoral
condyle (Fig. 27-4). The fascia lata is incised longitudinally in line with the
skin incision. The posterior part of the vastus lateralis muscle is exposed by anterior
retraction of the muscle and dissection along the fascia posteriorly to the
linea aspera. The muscle and fascia are split about 1 cm lateral to the linea
aspera. The perforating branches of the profundus femoris artery are identified
and ligated. These vessels course perpendicular to the long axis of the femur
at intervals of about 3 cm. The periosteum is split and elevated anteriorly
along the vastus lateralis muscle. Only a minimal amount of periosteal
stripping and muscle elevation should be performed. The intermuscular septum
should not be dissected off the linea aspera unless it is imperative for
surgical exposure. This lateral approach to the shaft results in minimal
scarring of the quadriceps and can be reused in future surgery on the shaft as may
be indicated.
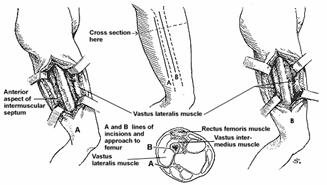
Fig.
27-4 Abord lateral si posterolateral 13 medie coapsa. A.Abordul
posterolateral de-a lungul septului intermuscular este preferat deoarece este
minima disectie prin vastul lateral. B. Abordul lateral cu incizia
vastului lateral si intermediar de-a lungul fibrelor
MECHANISMS OF INJURY
A fracture of a
normal femoral shaft requires major trauma. Most fractures are sustained by
young adults during high-energy injuries such as motor vehicle accidents,
auto-pedestrian accidents, motorcycle accidents, falls from heights, or gunshot
wounds.
Epidemiologic
studies show a correlation between the mechanism of injury and the types of
associated injuries.343 Auto-pedestrian accident victims have a high prevalence
of head, chest, pelvis, arm, and leg injuries. Motorcyclists tend to sustain
associated pelvis and ipsilateral leg injuries. Fall victims less frequently
sustain major associated injuries.343 Lesser degrees of trauma can fracture a
femur with pathologic bone. Such pathologic fractures often start at the weak
metaphyseal bone at the ends of the femur and propagate into the shaft.
Fatigue
failure is a rare cause of fracture of the femoral shaft.273 Usually located in
the proximal or midshaft areas, fatigue or stress fractures occur mainly in
military recruits undergoing a marked and prolonged increase in physical
activity.
The
incidence of stress fractures of the femoral shaft in civilian populations
appears to be rising with the recent emphasis on physical fitness. Running
accounts for most such fractures, but they also have been seen after triathlon
events and aerobic dancing.90 Most runners report an increase in their training
during or immediately before the onset of their pain. Plain radiographs often
are normal, and radioisotope scans have proven to be the most sensitive tests
for the early detection of these injuries. Displacement of these stress
injuries can occur occasionally, but most heal with rest or substitution of
low-impact exercises such as cycling and aquatic exercise for running.
Like
most bones, the femoral shaft fails under tensile strain.109 The most common
mechanism of injury is bending load, resulting in a transverse fracture.
Higher-magnitude injuries cause varying degrees of fracture comminution. It has
been estimated that 250 Nm of bending movement are needed to fracture a normal
adult femoral shaft.183 Additional force is dissipated on the soft tissues.
Pathologic bones are prone to spiral fractures after minor torsional loads.
Such fractures rarely are comminuted or associated with severe soft-tissue damage.
CLASSIFICATION
No universally
accepted classification scheme exists for fractures of the femoral shaft. Most
investigators categorize fractures according to specific variables that
directly influence their preferred treatment. Such factors as soft-tissue
injury, geographic location, fracture geometry, fracture comminution, and
associated injuries are used most often in classifying these fractures.
Open
wounds occur less frequently with femoral shaft fractures than with tibial
fractures. Open fractures can be subdivided into the standard grades I, II,
IIIA, IIIB, and IIIC, according to the Gustilo-Anderson method.130,131 The
abundant soft-tissue coverage of the femoral shaft makes grade III, especially
IIIC, open fractures relatively uncommon.
The
interobserver agreement with the Gustilo-Anderson classification system for
open tibia fractures is only moderate to poor.54 A similar problem with its
reliability and reproducibility may exist for femoral fractures, although this
issue has not been studied. The definitive grading of the soft-tissue wound
should be delayed until thorough inspection and debridement of the soft tissues
and bone are completed.
Femoral
shaft fractures can be categorized geographically as proximal third, midshaft,
or distal third. Because the isthmus of the medullary canal usually is located
in the midshaft, distal-third fractures also are called infraisthmal fractures.
The variable anatomy of the medullary canal and the different mechanical
stresses in these three regions of the shaft influence the techniques and
results of intramedullary fixation.
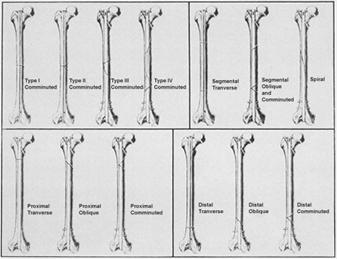
Fractures
also can be classified according to the geometry of the major fracture line.
The terms transverse, oblique, spiral, and segmental are self-explanatory. The
AO/ASIF classification distinguishes simple (A), wedge (B), and complex (C)
patterns in its scheme for femoral diaphyseal fractures240 (Fig. 27-5). The
simple fractures are subdivided according to the obliquity of the single
fracture line. The wedge fractures can be a spiral, bending or fragmented
configuration. The complex fractures include segmental fractures and fractures
with extensive comminution over a long segment of the diaphysis. It is unclear
how this AO/ASIF scheme may influence the preferred treatment of any given
fracture or be predictive of its outcome.
Fig.
27-5 Clasificarea ASIF
The
degree of fracture comminution has implications for the preferred form of
medullary fixation and locking of the major fracture fragments. The Winquist
classification of comminution is widely used369 (Fig. 27-6). Type I comminution
is defined as minimal or no comminution at the fracture site. Any small
fragment that is present should have no effect on fracture stability after
intramedullary nailing. Type II comminution involves a fragment larger than
that in type I but has at least 50% of the circumference of the cortices of the
two major fracture fragments intact. Because the broad cortical contact after
fracture reduction and nailing prevents shortening and malrotation, simple
intramedullary nails suffice for most type II fractures. Nevertheless, static
locking is used routinely for these type II injuries because of the risk of
postoperative loss of fixation secondary to unrecognized comminution.59

Fig.
27-6 Clasificarea Winquist: A. Tip I; B. Tip II; C. Tip III; D. Tip IV.
In
type III injuries, between 50% and 100% of the circumference of the two major
fracture fragments is comminuted. Such large butterfly fragments compromise
fracture fixation because broad cortical abutment of the major fracture
fragments is impossible. Simple intramedullary nails are insufficient for type
III fractures and must be supplemented with interlocking screws, cerclage
wires, or postoperative traction or bracing. All cortical contact is lost in
type IV injuries. The cortex is comminuted circumferentially over a segment of
bone. Even with intramedullary nailing, there is no contact between the
proximal and distal fragments. All inherent stability of the fracture is lost.
Longitudinal fractures with cortical fissures traversing the entire shaft
occasionally can be sustained with gunshot injuries.
Finally,
a patient can be categorized as having either an isolated femoral fracture or
multiple injuries. The presence of associated injuries often is the single
variable that determines the preferred timing for fixation of fractures of the
femoral shaft.254 The Injury Severity Score (ISS) is one of several scales used
to grade the severity of the multiply injured patient.19 Injuries to six body
regions (head and neck, face, chest, abdomen and pelvic viscera, extremities
and bony pelvis, and integument) are graded to quantify the extent of trauma.
Each area is assessed as mild (1), moderate (2), severe (3), critical-outcome
usually favorable (4), or critical-outcome usually lethal (5). The sum of the
squares of the three highest grades equals the ISS. The maximal score,
therefore, is 75.19,94 Retrospective studies show that the median lethal ISS
scores vary with the age group.126 The median lethal ISS score is 40 for
patients 15 to 44 years of age but drops to 29 for patients 45 to 64 years of
age and to 20 for patients 65 years of age and older.
SIGNS AND SYMPTOMS
The clinical
diagnosis of fracture of the femoral shaft usually is obvious, with pain,
deformity, swelling, and shortening of the thigh. A thorough physical
examination is imperative, however, because most fractures are a result of
high-speed trauma and associated injuries are common. Orthopaedic assessment of
the entire limb should be systematic and complete. The pelvic ring and hip are
inspected for tenderness. Swelling or ecchymosis may signal concomitant pelvic
disruption or hip fracture. Because the hip cannot be moved voluntarily by the
patient, palpation of the groin and buttock is important.81,278 Fullness of the
buttock with flexion and adduction of the proximal femur can denote a posterior
dislocation of the hip.
A
similarly thorough inspection and palpation of the knee should be performed.
Ligamentous injuries and internal derangements of the knee are commonly
associated with femoral fractures.234,267,323,352 Formal stress testing of the
ligaments is not feasible in the presence of a shaft fracture. Careful
palpation of the collateral ligaments and joint space, however, may raise the
index of suspicion for ligamentous injury, and clinical or radiographic stress
testing can be deferred until after femoral fixation.
The
precise prevalence of meniscal injuries associated with femoral shaft fractures
is unknown. In an arthroscopic study of the knees of 47 patients with closed
femoral shaft fractures, nearly half were found to have meniscal tears.352
Complex and radial tears outnumbered peripheral or bucket-handle tears. The
clinical significance of such tears remains unclear, however, and routine
arthroscopy of the knees of patients with femoral fractures probably is not
justified. Diagnostic assessment of persistent knee complaints should be
delayed until the completion of fracture rehabilitation of the limb unless
severe symptoms of locking and giving way are present.
Although
neurovascular injuries rarely are associated with closed shaft fractures, a
complete preoperative examination for vascular and neurologic damage is
mandatory. Because of the severe pain and spasm accompanying femoral fractures,
the motor strength of muscles below the knee may be diminished. Distal pulses
should be palpable.
Although
few patients with isolated fractures of the femoral shaft are in hypovolemic
shock, major blood loss into the thigh is present in most cases.361
In a
retrospective study of patients with isolated shaft fractures, Lieurance and
colleagues195 reported that 21 of 53 required transfusions and estimated the
average blood loss in all 53 patients to be more than 1200 mL. Therefore,
careful preoperative assessment of the hemodynamic stability of the patient is
necessary, regardless of the presence or absence of associated injuries.
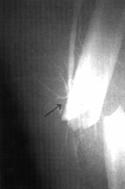
RADIOGRAPHIC FINDINGS
Before
diagnostic radiographic studies are performed, longitudinal traction or
splinting of the extremity is applied to ensure minimal additional soft-tissue
injury to the thigh. If a Thomas splint is used, the metallic ring and caliber
should not obscure any part of the bone. Nondisplaced fractures of the femoral
neck frequently are missed because of the overlying shadow of a splint or
inadequate quality of the preoperative radiograph (Fig. 27-7). If the hip is
externally rotated on the preoperative radiograph, there can be rotational
artifact. In such cases, it is advisable to obtain an anteroposterior
radiograph of the hip with the proximal femur internally rotated in the
anesthetized patient before the operative procedure.
Initial
radiographs should include an anteroposterior view of the pelvis and
anteroposterior and lateral views of the knee and the entire femur. Baseline
chest radiographs also are helpful in the event of the development of a fat
embolism syndrome. The quality of the femoral radiographs must be sufficiently
good to detect longitudinal cracks and nondisplaced comminution of the proximal
and distal fragments. Poor-quality radiographs also can disguise subtle
scalloping or erosion of the cortex, which may be the only sign of a pathologic
fracture. Such a fracture can be easily misdiagnosed as a traumatic injury to a
normal femur. Suboptimal radiographs should not be accepted.
TREATMENT
Nonoperative Techniques
Traction
Traction has
been the time-honored method of treating femoral shaft fractures and can be
divided broadly into skin traction and skeletal traction techniques. Skin
traction encompasses those traction modalities that apply longitudinal force to
the limb through the skin. Skeletal traction includes all traction designs that
apply force to the limb directly through the skeletal system, most often
through a percutaneous pin in the tibia or femur.
Centuries
ago, De Chauliac and coworkers100 suggested the concept of skin traction on the
leg with the knee in extension for fractures within the thigh. Their method was
modified in the 1860s by Buck,64 whose name is still associated with this form
of traction. The major disadvantage of skin traction is the inability to apply
sufficient forces to the limb to obtain fracture reduction. The application of
major force can cause slippage of the skin traction or skin necrosis.
Furthermore, because of the deforming muscle forces on the proximal and distal
fragments, displacement of the femoral shaft fracture commonly occurs when the
knee is held in extension.78 Other methods of skin traction, including Bryant
and split Russell303 traction, have been suggested to counteract these
disadvantages. These traction techniques are indicated only in young children.
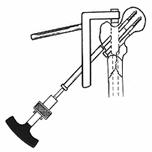
Although
it is recognized that skin traction cannot supply a constant force of
sufficient magnitude to maintain length and alignment of femoral shaft
fractures in the adult, it is still used in emergency immobilization and
transport of the patient who has sustained a lower extremity injury. In this
situation, the fractured femur is splinted with traction applied through a
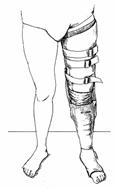
padded wrap around the foot and heel with countertraction in the groin (Fig.
27-8). Limb rotation is controlled through multiple elastic straps that
circumferentially encase the thigh. This technique greatly decreases patient
discomfort and facilitates patient transfers in the prehospital and emergency
department settings. However, it should always be considered a temporary
measure. Definitive techniques to restore the fractured femur to length and
alignment should be planned and executed as soon as the patient's condition
permits. Because extensive thigh swelling can cause the elastic straps
surrounding the thigh to act as tourniquets, the tension of the traction and of
the thigh straps should be checked and appropriately adjusted once patient
transfer is complete.
Skeletal
traction, the most common method of definitive treatment of femoral shaft
fractures for decades before the 1970s, remains the method of choice for early
fracture care. Sufficient force can be applied to the limb to achieve fracture
reduction. The skeletal traction pin most commonly is inserted through the
tibial tubercle, a relatively subcutaneous area anatomically removed from the
knee joint and not contiguous with the fractured bone. However, proximal tibial
skeletal traction may be contraindicated when ligamentous injury to the
ipsilateral knee accompanies the femoral shaft fracture.
The
distal femur has been used successfully for skeletal traction and offers more
direct longitudinal pull on the fractured femur than does similar traction
through the proximal tibia. Theoretically, infection of a distal femoral
traction pin could involve the knee joint, but this complication has not been
identified as a serious clinical problem. Skeletal traction through the distal
femur has been associated with a higher rate of knee stiffness after fracture
union, undoubtedly because of pin-tract scarring of the vastus medialis and
vastus lateralis. The orthopaedist treating traumatic injuries should be facile
at skeletal traction pin insertion at both sites.
Debate
has continued over which type of traction device, the Kirschner wire or the
Steinmann pin, is superior for skeletal traction. Charnley and Guindy80
expressed a preference for the Steinmann pin, believing that its larger
diameter provides better fixation, especially in osteopenic bone. They argued
that the Kirschner wire has two definite disadvantages: (1) every movement of
the traction bow with a Kirschner wire is transmitted to the bone, permitting rotation
at the bone-pin interface, and (2) the wire can cut through the bone and
subsequently loosen. Other authors recommend the Kirschner wire over the
Steinmann pin because the former is a smaller device and, thus, creates less
soft-tissue damage on insertion.231 They also believe that, with traction, the
Böhler bow connections to the Steinmann pin fail to swivel, creating rotation
of the pin within the bone. Although the best traction is a matter of surgeon's
preference, it is agreed that threaded pins should not be used because they are
weaker than smooth pins of the same diameter.231
Appropriate
sterile technique, including skin preparation and towel draping, and local
anesthesia are mandatory for pin insertion. The proximal tibial skeletal
traction pin is inserted at the level of the tibial tubercle. Pin insertion
through the dense anterior cortex of the tibia should be avoided because
bicortical pin placement is preferred. Thermal necrosis of the anterior cortex
of the tibial crest also can result in pin-tract infections.
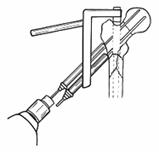
Many
variations of limb suspension for traction on the fractured femur have been
devised; most are modifications of the Thomas splint with the Pearson
attachment. This type of balanced skeletal traction has replaced the fixed
splinting devices such as the Böhler-Braun frame78 (Fig. 27-9). The half-ring
of the Thomas splint fits loosely around the upper thigh. Slings support the
thigh, helping to prevent soft-tissue and bony sag through gravity. Traction is
applied in the general line of the femur, and the foot is supported in the
Pearson attachment.277 The Thomas splint and the Pearson attachment are
suspended by traction ropes to support the lower limb, hence the term balanced
skeletal traction. Adjustments in limb rotation and alignment are possible with
the use of secondary slings. Charnley79 has provided a complete description of
the technique of fracture reduction and alignment. This technique permits early
function of the thigh musculature and some early knee motion. Emphasis on early
knee motion by Delorme and associates,102 Hogden,145 and Perkins67 brought
about further modifications of this classic design.
Another
variation, Neufeld traction,53,116,213 incorporates the limb and the Steinmann
pin in plaster casts and applies traction through a roller system that permits
greater early knee motion (Fig. 27-10). Traction is placed on the plaster cast,
which transfers this force to the bone through the incorporated Steinmann pin.
The increased knee motion permissible with Neufeld traction has not led to an
increase in fracture nonunion. Alterations of this method can permit increased
patient mobility, because the patient can have continuous traction while being
positioned on either flank. In addition to permitting the maximum amount of
knee motion and muscular activity of any traction technique, this method may
allow improved pulmonary toilet in the multiply injured patient. Most skeletal
traction methods require that the patient remain in the supine position.

Fig. 27-10
Exista doua linii - pt
tractiune
si pt suspensie. De notat
folosirea
tensiunilor variabile prin
modificarea
pozitiei carligului
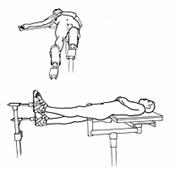
Finally,
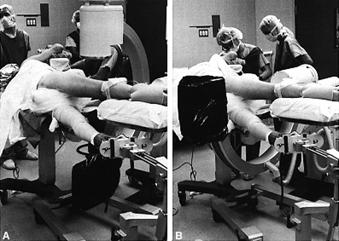
90-90 traction is so named because the hip and knee each are positioned in 90°
of flexion225,247 (Fig. 27-11). This method is applicable to more proximal
femoral shaft injuries, especially those extending into the subtrochanteric
region, in which flexion of the proximal fragment occurs. The foot is
incorporated in a plaster cast or supportive sling, and the traction pin routinely
is inserted through the distal femoral condyles. Countertraction is provided by
the patient's own body weight. This technique affords excellent access to
wounds in the posterior thigh. Circulatory compromise in patients with
peripheral vascular disease can occur with this method, so it is not
recommended for elderly patients. Knee subluxation with proximal tibial 90-90
skeletal traction has complicated this technique.225

Fig.
27-11 Tractiunea 90-90 utila in fracturi subtrohanteriene, leziuni inghinale
si ale fetei posterioare a coapsei. Tractiunea condililor
femurali este mai eficienta. Suspensia gambei intr-un gips este de-obicei
necesara.
One
early goal of skeletal traction is to restore the fractured femur to proper
length within the first 24 hours after injury. After that time, the fracture
hematoma begins to organize, and pulling the fracture out to normal length
requires increasing amounts of traction. These increasing traction forces can
cause the patient to be pulled toward the end of the bed, often resulting in
abutment of the patient or the traction equipment on the foot of the bed.
Inadequate traction and failure to restore the fracture to length can result.
Multiple radiographs should be taken to determine the efficacy of the traction
in the first 24 hours after its application, because slight fracture
distraction is preferred over continued overriding of the fracture fragments.
It is not unusual to place 30 to 40 lb of traction initially, only to need
diminished amounts later.
Before
the 1970s, skeletal traction therapy was continued for a patient until
significant radiographic and clinical evidence of fracture union was apparent,
usually requiring a minimum of 6 weeks of in-hospital care. A unilateral
weight-bearing spica cast then was applied, and the patient began to ambulate
with progressive weight bearing. The spica cast was removed 3 to 6 months after
injury, and range-of-motion exercises of the ipsilateral hip and knee were
begun.
The
results of traction therapy for fractures of the femoral shaft have been
acceptable.103,236 Most studies report the rate of union of closed fractures of
the femoral shaft treated with skeletal traction to be between 97% and 100%.67
However, delayed union has occurred in up to 30% of cases, possibly from
continual distraction of the fracture site.70,247 Control of limb length is
difficult, especially in comminuted injuries, with frequent shortening of 1 to
3 cm reported.103,313 Rotational malalignment generally has been attributed to
maintenance of the foot pointed toward the ceiling. Such positioning with the
patient supine in bed results in internal rotatory malalignment of the distal
fragment.
Knee
stiffness is the most common clinical problem after prolonged traction
therapy.69,299 In a study by Winant,367 no patient regained full knee flexion
and only 47% regained more than 90° of knee flexion. Loss of knee flexion has
been noted by several other investigators as well,67,103,118 although some
document return of the knee's full range of motion in many patients. Despite
the mixed results with traction treatment, it is clear that rotational
deformity, loss of range of knee motion, and limb-length discrepancy can be
well tolerated by many patients.236 However, other areas of concern persist.
The required lengthy hospitalization, prolonged recumbency, and major cost of
traction treatment remain serious problems.69 In the last few decades, the
detrimental effects of traction therapy as opposed to early operative fixation
of femoral shaft fractures have been documented. Major patient benefits are
derived from early fracture stabilization and patient mobilization. Therefore,
the enthusiasm for skeletal traction treatment has waned over the years in
favor of surgical techniques.
There
is no doubt that traction historically has been the treatment method of choice
for femoral shaft fractures.268 It has been used successfully in both closed
and open injuries for decades and remains the least invasive treatment method
for these injuries. Knowledge in this area is still required for the
application of traction as a temporary method of stabilization before and
during more modern internal fixation procedures. Although the treatment of
femoral shaft injuries has shifted to an operative approach in the last few decades,
patients occasionally must still be treated definitively with traction.
Cast Brace
The development
of cast brace systems was motivated both by a desire for ambulatory treatment
and by a need to prevent the hip and knee contractures that were frequent
sequelae of spica cast treatment. The cast brace is essentially an external
support device that has several theoretic advantages. It permits progressive
weight bearing, which leads to graduated functional improvement in the muscles
and joints and to increasing skeletal stresses that stimulate fracture healing.
It works by partial unloading of the fracture through circumferential support
of the soft tissues by a smooth, total contact plaster or plastic thigh cuff
(Fig. 27-12).
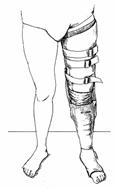
Fig.
27-12
Although
the precise effect of a cast brace on fracture loading depends on several
variables, including fracture location and anatomy, soft-tissue coverage, and
contouring of the thigh plaster, several of its mechanical properties are well
defined.232 The fracture itself controls loading in a cast brace.219 Most cast
braces carry loads of only 10% to 20% of body weight and function mainly as
antibuckling hinged tubes. The major deformation counteracted by the cast brace
is lateral angulation produced by the thigh musculature. Once telescoping of
the thigh has ceased, the muscles provide little hydraulic support to the
fracture. Electrogoniometer and cineroentgenography studies demonstrate that
sizable translation of the fracture occurs with weight bearing.92 This motion
progressively decreases as fracture healing proceeds.
Open
fractures, distal-third fractures, and comminuted midshaft fractures are
relatively good indications for cast bracing.92,229 Proximal shaft fractures
and simple transverse or oblique fractures are less amenable to cast bracing
because of their high stress concentration and tendency toward angulation. Cast
bracing also can be used to supplement limited internal fixation of shaft
fractures, such as with small-diameter nonlocked intramedullary nails.321 Its
function in such applications is primarily to neutralize torsional loads on the
femur that might lead to rotational malalignment of the fracture. The technique
of cast bracing is well described in many publications.188,219,231,232 Careful
application is critical for success. It can be used as a substitute to hip
spica casting after 6 to 8 weeks of traction or as a primary treatment after 1
to 2 weeks of traction. The timing of application should be dictated by the
experience of the treating orthopaedist and the likelihood of loss of reduction
of any given fracture. A prerequisite of cast bracing is that satisfactory
reduction in traction be achieved before the cast is applied. The best results
are obtained when the cast brace is applied after pain and swelling have
subsided and early callus formation is evident on radiographs. Serial
radiographs are imperative to check the alignment and judge the advisability of
early weight bearing.
The
goals of early limb rehabilitation and rapid fracture healing can be realized
in most patients. Most investigators report a consistently high rate of union,
usually by 13 to 14 weeks after injury.137,215,231,232,321 However, major
complications haunt most cast brace systems. Femoral shortening, averaging 1 to
1.5 cm in even the best of series, often requires corrective shoe lifts at the
completion of treatment. Varus angulation of more than 5° to 10° results in
excessive loading of the medial compartment of the knee and cosmetic deformity.
Although knee motion with cast bracing often is described as good,
well-documented series of patients treated by cast bracing reveal residual knee
motion at follow-up of less than 100°.215,231 The prevalence of these
complications is especially high in the hands of physicians who use cast
bracing infrequently. Various modifications of the standard plaster cast brace,
such as adjustable thigh sections, pelvic belts for suspension, and improved
hinges, have been recommended to address these common problems.92,188
The
popularity of cast bracing peaked many years ago, and it has been largely
supplanted by newer techniques of internal fixation. However, it should still
occupy a place in the armamentarium of fracture surgeons for the management of
fractures of the femoral shaft.
Operative Techniques
External Fixation
External
fixation using percutaneous pins inserted proximal and distal to the fracture
gained initial popularity for the stabilization of fractures of the femoral
shaft during World War II. This method provided excellent bony fixation and
wound access as well as permitted early patient ambulation. However, it was
extremely controversial at the time, with some authors reporting excellent
results but others publishing high rates of nonunion, pin-tract infection, and
knee stiffness.230
The
pins of external fixators often tether the quadriceps muscle to the femoral
shaft. The resultant scarring can cause a permanent loss of motion of the knee.
This problem was compounded with early external fixation designs that used
transfixion pins that exited the thigh on both the medial and lateral
surfaces.166,249 There remain few, if any, indications for the use of
transfixion pin frames for fractures of the femoral shaft. The lateral half-pin
external fixator designs, pioneered by Wagner,319 have been shown to provide
adequate bone fixation and stabilization for most complex femoral shaft
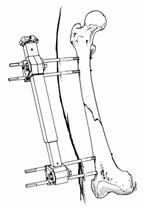
injuries84,98,99,123,154 (Fig. 27-13). As with other long-bone stabilization,
the rigidity of femoral external fixators depends mainly on the pin diameter.84
As long as a half-pin at least 5 mm in diameter is used, adequate stiffness of
nearly all commercially available frames can be achieved. Laterally placed
frames are stiffest in the mediolateral plane, whereas anteriorly placed frames
are stiffest in the sagittal plane.
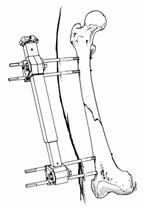
Fig.
27-13
Published
series of external fixation of the femur report mixed results. Some authors
have judged that the return of 90° of knee flexion is an acceptable result and,
therefore, report a high percentage of excellent functional outcomes with this
technique.98,156,319 Other investigators have reported decreases in the
functional range of motion of the knee at follow-up.11,125,156 These
differences are due to many factors, most notably the method of pin insertion,
the number and type of external fixation pins, and the severity of the
soft-tissue injury accompanying the fracture.
One
comparative study between external fixation and interlocking intramedullary
fixation for closed fractures of the femoral shaft disclosed distinctly
superior clinical results with the intramedullary technique, although the
severity of injuries between the two treatment groups was not identical.241 The
high rate of fracture union was equivalent in the two groups, but the external
fixation group had complications of knee stiffness and pin-tract infection.241
Pin-tract
infection complicates up to 50% of the reported cases of external fixation of
the fractured femur, undoubtedly because of pins traversing the iliotibial band
and the broad muscle belly of the vastus lateralis. This complication must be
accepted as a routine problem inherent with the use of this method. Although it
can be lessened with good pin insertion technique, it cannot be
eliminated.46,99,125,132
External
fixation of the femoral shaft reportedly has been used most often in
high-energy injuries in which rapid, rigid fracture stabilization is required
because of the patient's associated injuries.48 Today, the major indication for
using external fixation for the femoral shaft is grade III open fractures (Fig.
27-14). This technique provides adequate bony stabilization, even in comminuted
injuries, and permits excellent wound access for debridement and dressing
changes. In the severely contaminated or high-energy open fracture, external
fixation is the treatment of choice because the risk of infection with internal
fixation can be prohibitive. The slightly increased prevalence of fracture
nonunion and decreased range of motion of the knee reported with this technique
may be due, in part, to the severity of injuries studied.99,156 No controlled
studies exist that compare the results of similar injuries treated with
external fixation and other treatment methods.
Circular
or small-wire external fixators (Ilizarov) used in limb lengthening and the
correction of post-traumatic deformity obstruct access to the thigh for the
multiple debridements and dressing changes required with these grade III
fractures and, thus, are poor choices for initial fracture treatment. If these techniques
are required later, previous external fixation with half-pin frames does not
preclude their use.
Because
intramedullary nailing techniques have demonstrated more predictable fracture
healing and improved clinical results with closed injuries, external fixation
is not indicated in the routine treatment of closed fractures of the femoral
shaft.241 In certain clinical situations, such as the multiply injured patient
who cannot tolerate prolonged anesthesia or the patient with a closed fracture
of the femoral shaft and an associated vascular injury,285 external fixation
may be the safest and most expedient method with which to stabilize the
fracture. In these instances, it usually is considered as temporary fixation
and is replaced by internal fixation once the emergency situations have been
resolved.11,48 However, caution should be exercised if the external fixator is
used as a temporary fixation device.11 The prevalence of infection in the femur
after internal fixation (either plate or intramedullary nail) following the
removal of an external fixator is unknown. Caution should be exercised in
internally fixing a fracture in the presence of colonized pin tracts of a
temporary external fixator.
Plating
During the 1960s
and 1970s, the treatment concepts of rigid internal fixation of diaphyseal
fractures followed by early limb rehabilitation gained wide acceptance.
Dissatisfaction existed with the results of nonoperative treatment of femoral
shaft fractures because of the prolonged hospitalization, high costs, fracture
shortening, malunion, delayed union, and joint stiffness reported with these
methods.103,137,247,318 Open reduction with plating of femoral shaft fractures
was espoused in an effort to improve these results, and the clinical results of
plating compared favorably with those of closed treatment or limited internal
fixation.300
This
technique requires experience and operative skill to anatomically restore the
alignment of a comminuted femoral shaft fracture without further devitalizing
the fracture fragments through dissection. Evacuation of the fracture and at
least partial devascularization of the femoral cortex are inevitable with
plating of the fracture. Some authors apply plating to all fractures of the
femoral shaft,82,287,300,330 whereas others limit its use to those fractures
that are not amenable to intramedullary nailing, with or without cerclage
wiring.160,271,291,330 The goal of the operative procedure is fracture
stability. Early in the history of plating of femoral fractures, multiple
plates were applied to the femoral diaphysis to obtain more secure fixation.
These were referred to as 90-90 plates, because they were applied 90° from one
another on the anterior and lateral cortices to enhance rotational
stability.209,271,300 Improvements in plate strength and design permitted
fracture site compression and allowed single plating of fractures of the
femoral shaft. Less surgical dissection is required with single compared with
double plating.203,330
Open
reduction and plating overcome the difficulties encountered with skeletal
traction with respect to the restoration of femoral length and rotational
alignment. Direct visualization of the fracture fragments facilitates an
anatomic or near-anatomic reduction. This technique improves the range of
motion of the knee, compared with the results obtained with skeletal
traction.82,203 This improvement is attributed to both the rigid fixation
achieved with the compression techniques of the ASIF group and early
rehabilitation of the limb. However, despite this clinical improvement, 20% to
30% of patients still have major residual loss of knee motion, generally
attributed to excessive scarring of the quadriceps muscle.246,348 Careful
dissection of the vastus lateralis muscle combined with early postoperative
knee rehabilitation can minimize knee contracture.287
Another
advantage of this technique is prompt mobilization of the patient with a
shorter hospital stay compared with that required for skeletal traction. The
benefits of immediate stabilization of long-bone fractures on pulmonary
function were recognized only after open reduction with internal fixation of
femoral shaft fractures was studied.
Although
this method addresses some of the problems encountered with skeletal traction
treatment, an array of new complications has become apparent. Failure of
fixation occurs in 5% to 10% of the reported cases, with many requiring
reoperation.4, 160, 203, 286, 291, 300, 330 Fixation failure more than 6 months
after surgery indicates a nonunion. Fatigue fracture of the plate can be
salvaged easily in most cases by intramedullary nailing of the nonunion.286
The
prevalence of infection is higher with plating of fractures of the femoral
shaft than with conservative treatment methods or closed intramedullary
nailing.18,160,216,246,336 Devitalization of fracture fragments naturally
occurs with injury. However, further iatrogenic tissue and bone necrosis can
occur with the dissection for open reduction, a variable dependent on the care
and experience of the surgeon. Tissue necrosis from excessive dissection can
create an environment that is less favorable for fracture union and more
favorable for infection after surgical contamination.330 Most studies
concerning plating of femoral shaft fractures demonstrate overall rates of
healing between 90% and 95%.203,300,330 This figure is decreased somewhat when
open fractures are added to the investigation. Infection has complicated zero
to 11% of the reported cases.109, 134, 148, 190, 207, 228, 342 Ruedi and
Luscher300 reported a large series (126 comminuted fractures over 6 years) of
femoral shaft fractures treated with open reduction and plating. Although they
reported 92% good or excellent final results, 9% of cases lost fixation because
of nonunion, 9% required bone grafting for delayed union, and 6% became
infected. Most of these complications required reoperation. These authors
strongly recommended routine bone grafting of comminuted femoral shaft injuries
treated with open plating.300
In a
more recent series, Riemer and colleagues286 reported improved results when
minimal dissection and routine bone grafting were used. Of 141 fractures
treated with a single AO large-fragment plate and cancellous bone grafting,
only ten plates failed and only one surgical wound infection was recorded.
Fracture union occurred at an average of 17.2 weeks. Despite excellent final
knee motion in nearly all cases, rehabilitation was slow in most patients.
Contraindications to plating in the multiply injured patient were considered to
include coagulopathy, preexisting skin infection, cardiac instability, and
severe head injury with uncontrollable and fluctuating intracranial pressure
measurements.
This
technique requires an extensive surgical exposure of the lateral aspect of the
femur. The entire leg is draped free with the patient positioned at the
ipsilateral edge of the operating table. The vastus lateralis muscle is
reflected anteriorly with ligation of the perforating vessels, and the major
proximal and distal fragments are mobilized sufficiently to obtain an anatomic
reduction. Ten- or 12-hole dynamic compression plates with a minimum of five
screws in both the proximal and distal fragments are used routinely. Bone
forceps hold the plate to the bone without additional elevation of the muscles.
A minimal number of intrafragmental screws (preferably through the plate) are
inserted to prevent excessive damage to the soft tissues. All medial cortical
defects are grafted, and large suction drains are inserted deep in the wound.
Perioperative antibiotics should be used to minimize the chance of
infection.348
Active
range of motion exercises for the knee are encouraged soon after surgery, but
forceful strengthening exercises are avoided until fracture healing is evident.
Full weight bearing is postponed until complete radiographic union is present.
This delay in weight bearing for 3 to 5 months is a major disadvantage of
plating compared with closed reamed intramedullary nailing.
The
popularity of this technique has decreased since its peak in the early
1970s.112,115 With the advent of improved intramedullary techniques in the
1980s, open reduction and plating no longer was considered the preferred
treatment option for femoral shaft fractures. Interlocking nailing controls
femoral length and rotation without the risks of tissue devitalization,
quadriceps scarring, blood loss, and infection from plating. The only remaining
advantage for open reduction inherent to this open plating technique over
closed intramedullary nailing is that open plating does not require the wide
spectrum of specialized operating room equipment and radiology personnel that
are necessary for closed intramedullary nailing.
 Because the clinical results with interlocking nailing
are superior to those with open reduction, few indications remain to treat a
fracture of the femoral shaft with open plating. Fractures that involve the
distal metaphyseal-diaphyseal junction of the femur still may require extensive
open reductions, especially when intercondylar extension is present (Fig.
27-15). An 'indirect reduction' technique has been advocated by the
ASIF group to obtain fracture stabilization of these complex injuries without
excess dissection, surgical manipulation, and anatomic reduction of the
comminuted fracture fragments.33,210,287 Further study of this surgical
technique is necessary to see whether it affords decreased rates of nonunion
and infection when compared with previous open reduction methods (Fig. 27-16).
Because the clinical results with interlocking nailing
are superior to those with open reduction, few indications remain to treat a
fracture of the femoral shaft with open plating. Fractures that involve the
distal metaphyseal-diaphyseal junction of the femur still may require extensive
open reductions, especially when intercondylar extension is present (Fig.
27-15). An 'indirect reduction' technique has been advocated by the
ASIF group to obtain fracture stabilization of these complex injuries without
excess dissection, surgical manipulation, and anatomic reduction of the
comminuted fracture fragments.33,210,287 Further study of this surgical
technique is necessary to see whether it affords decreased rates of nonunion
and infection when compared with previous open reduction methods (Fig. 27-16).
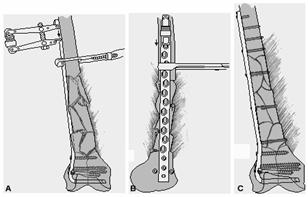
Fig.
27-15
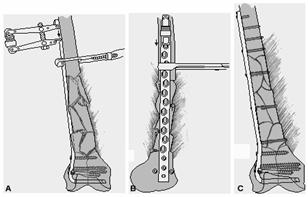
Fig.
27-16A+B. reducerea indirecta a unei fracturi cominutive in 13
distala. Se practica minima disectie a fragmentelor
cominutive. Dupa reducerea anatomica si fixarea fragmentelor
intraarticulare se aplica lama placa 95 grade pt a obtine reducerea
fragmentelor diafizare. Sistemul de compresie ASIF se aplica invers
folosindu-l la refacerea lungimii femurului. C. Incidenta AP cu OS
finala cu lag-screw de mentinere a fragmentelor mari. Succesul
acestei tehnici depinde de minima disectie a zonei diafizare
faracu minima devascularizare a fragmentelor osoase cominutive.
Intramedullary Nailing
The straight,
tubular anatomy of the femoral shaft is ideally suited to intramedullary
fixation. The centrally located isthmus allows for endosteal purchase both
proximally and distally by an intramedullary rod. The loading conditions of the
femur by gravitational, muscular, and ligamentous forces also are favorable for
intramedullary fixation.9 The femur normally is loaded in compression, bending,
and torsion. Both bending and torsion loads generate a combination of tensile,
compressive, and shear stresses in the bone. Compared with other internal and
external devices, such as plates and external fixators, intramedullary nails
are closer to the center of motion of the body and, thus, are subjected to
lesser loads. In addition, in fractures stabilized with cortical contact of the
major proximal and distal fracture fragments, the bone share of loading
increases as healing progresses. This mechanical property of the nail-bone
composite is distinctly different from the load shielding inherent with plate
fixation and has several beneficial effects. First, the intramedullary nail is
loaded less than a plate, making it less likely to fail in fatigue. Second, the
fracture callus is loaded progressively, stimulating healing and remodeling.
Finally, the cortical osteopenia usually evident from the stress shielding of
plates is avoided with intramedullary implants.
Intramedullary
nailing has many theoretic and practical advantages over the other forms of
internal and external fixation. Although specialized instrumentation and
radiographic facilities are needed for closed nailing, nails are inserted with
relative ease without the extensile exposures and dissection required for plate
application. Because the fracture hematoma is not evacuated with closed
nailing, the early action of local cellular and humoral agents critical to
normal fracture healing is not disturbed (Fig. 27-17). Therefore, closed
nailing constitutes a form of 'biological' fixation of the femur. The
lesser surgical dissection carries the added benefits of a lower infection rate
and less quadriceps scarring.
Intramedullary
nails provide predictable restoration of shaft alignment. In simple midshaft
fractures, large-diameter nails that fill the medullary cavity automatically
correct the normal alignment of the femur. Similar restoration of anatomic
length and alignment is possible with comminuted fractures and those proximal
or distal to the midshaft but requires more technical precision.
Early
functional use of the extremity is feasible after most cases of intramedullary
nailing. Patient mobilization out of bed within 24 hours of surgery is the
norm. As load-sharing implants, nails allow for early weight bearing after most
fractures. Only severely comminuted and distal shaft fractures may require
protected weight bearing during the early stages of fracture healing. The
minimal surgical scarring of the thigh musculature after nailing enhances early
recovery of quadriceps function and knee motion. This rapid rehabilitation that
is normally evident after nailing decreases the length of hospitalization and
the total period of disability, yielding obvious economic benefits.
The
rapid fracture healing that occurs after intramedullary nailing can be
attributed to several factors. Nails allow cyclic compressive loading across
the fracture site, which has a propitious effect on callus formation and
remodeling. The closed insertion of nails causes little or no damage to the
periosteal vasculature, which plays a dominant role in fracture healing. In
addition, marrow elements and cortical reamings extravasate into the fracture
hematoma during closed nailing. Such reamings serve as osteogenic,
osteoconductive, and, perhaps, osteoinductive stimuli to fracture healing.83
Thus, biomechanical and biological factors combine to create an excellent
milieu for the healing of shaft fractures after closed nailing.
Nailing
also is associated with a lower prevalence of refracture than are other forms
of internal and external fixation. Shaft fractures after closed nailing
predictably heal with abundant callus formation and little or no osteopenia of
the major fracture fragments. Because of the greater diameter of the callus and
the neocortex at the fracture site, the strength of the bone actually may be
greater than normal. Although nail extraction routinely is not recommended for
18 months, safe removal as early as 6 months is possible in selected young
adults because of rapid healing and remodeling. No protection in the form of
casts or delayed weight bearing is necessary after nail extraction.56
Specific
clinical studies comparing the results of intramedullary nailing with other
nonoperative and operative treatments consistently have demonstrated the
superiority of intramedullary fixation. The data show fewer cases of malunion,
improved function, earlier return to work, shorter hospitalization, less
fracture shortening, and more rapid healing with intramedullary nailing.70,163
Fewer complications of treatment occur, except for those related to infection
after open nailing.
The
history of intramedullary nailing of femoral shaft fractures is long and rich.
Fifty years after Küntscher's revolutionary work on intramedullary fixation,
his cloverleaf nail remains the benchmark for intramedullary implants. The
original Küntscher nail had a V-shaped cross-sectional design that was modified
to the current cloverleaf shape as instrumentation was developed for its closed
insertion over a guide pin. Many additional refinements in the Küntscher system
have been introduced over the years, but the basic concept and system remain
unchanged.
The
Küntscher nail served as the impetus for the development of many other nails.
These alternative intramedullary rods and nails have not consistently
reproduced the outstanding results of the Küntscher nail. The Rush rod, first
applied in the 1930s to femoral shaft fractures, is a curved, round pin that is
inserted in such a fashion as to create a dynamic force within the bone.302
Proper application of the Rush rod requires an accurate assessment of the
muscular forces on the bone with an attempt to oppose these intrinsic forces
with the bent rod. Similar flexible fixation is achieved with Ender pins.106
These thin, stainless steel rods, originally designed for peritrochanteric
fractures, have been widely used for shaft fractures. They can be inserted
through either the greater trochanter or the femoral condyles, depending on the
location of the fracture. Although satisfactory results are obtainable for
simple transverse and short oblique fractures and for fractures with
unicortical comminution, complex patterns involving long oblique, spiral,
distal, and comminuted fractures tend to shorten over the pins. Adjunctive
fixation in the form of cerclage wires, limited plate fixation, external
fixation, cast bracing, or postoperative traction may be required.257,258 When
adequate fixation is achieved, healing occurs rapidly.
The
Rush rod and Ender pin systems have numerous problems. As internal splints,
they provide little resistance to axial loads. Postoperative shortening and
malalignment are common, especially in complex fractures.164 Despite techniques
such as stacking multiple nails in the canal and diverging the rods in the
proximal and distal fragments, the anatomic results have been poorer than those
of interlocking nails. Rod irritation and resultant knee or hip pain may
necessitate early implant removal. Because of the inherent design and technical
problems with these small-diameter rods, they seldom are used for the treatment
of shaft fractures in adults. Some authors recommend that they be used only in
patients with femora with small medullary canals (á8 mm), in fractures below
noncemented femoral prostheses, or in fractures in young children requiring
intramedullary fixation that avoids open physeal plates.144 However, the
efficacy of Ender nails in such selected cases has not been proven.
Two
noncannulated nails have been widely used in North America. The Hansen-Street
diamond-shaped nail has a tapered end and, thus, can be inserted with or
without reaming.146 The flanged Schneider nail incorporates the double I-beam
principle in its design and is very strong. The four flanges along the length
of the nail provide improved rotational control of the fracture fragments. The
graduated sawtooth configuration of the ends of the nail acts as a self-broach
during its insertion without prior reaming. Either antegrade or retrograde
insertion is possible. Both the Hansen-Street and the Schneider nails are
intended for use without guide pins. Although excellent results are reported
for these nails in simple fractures, their usefulness is limited in more
complex injuries311,337 (Fig. 27-18).

Fig.
27-18 Telescoparea unei fracturi oblice in 13 medie in jurul unei tije
Schneider nealezata. Cele 7 grade de varus se atribuie punctului lateral
de intrare al tijei la nivelul trohanterului precum si localizarii
proximale a fracturii.
The
Samson fluted rod was designed specifically to strengthen the nail and improve
its rotational fixation of fractures. It possesses a closed, circular
cross-sectional configuration with circumferential external flutes that cut
into the endosteal cortical surface. A system of extenders that attach to the
end of the nail precludes the need for a large inventory of various-length
nails. Compared with other nails of comparable diameter, the bending strength
of the Samson nail is 40% to 80% greater and the torsional rigidity is 230% to
3000% greater.10 The nail was developed mainly for comminuted fractures and cases
of nonunion in which resistance to torque is critical for successful healing.
In one report, postoperative loss of rotatory alignment of 20° to 30° occurred
in six patients with comminuted fractures.127 Early weight bearing should be
deferred in fractures with Winquist III or greater comminution. Although good
results are attainable with this implant, its stiff properties increase the
risks of comminution of cortical bone during its insertion. Overreaming of the
canal by several millimeters often is necessary to prevent such comminution.
This very stiff nail also can stress-shield the fracture and retard normal
healing. More flexible, slotted nails have supplanted the fluted nail at most
centers.
The
Huckstep nail was designed mainly for use in unreliable patients in Third World countries.152,153 It is a very strong square nail with 4-mm holes drilled every
1.5 cm along its length. Locking screws inserted through targeting jigs can
stabilize comminuted fractures. The stiffness of the nail in torsion, bending,
and tension is much greater than that of most other commercially available
nails. Despite many improvements in its design over the last 15 years, its use
is still limited.
The
Küntscher cloverleaf nail is the most popular nail in general use. Although
minor modifications, such as tapered ends, closure of the slot, and placement
of locking holes, have been developed, the basic design has remained unchanged
over 50 years. The cloverleaf configuration permits closed insertion over a
guide pin. The longitudinal grooves of the nail also permit reconstitution of
the endosteal vasculature. The slot in the Küntscher nail decreases its
torsional rigidity. The nail tends to compress circumferentially as it is
driven into the canal. Küntscher believed that the elastic rebound of the nail
on the endosteal surface was responsible for rigid fixation. Such elastic
impingement does occur to a minor extent, but the fixation of most Küntscher
nails is due to their multiple sites of contact over a long segment of the endosteum
of the proximal and distal fragments.
Although
the original Küntscher nail was straight, most current designs are prebent for
the antecurvature of the femoral shaft. The prebent design eases nail insertion
and minimizes posterior gapping and distraction of the fracture site.
The
Küntscher nail can be inserted without reaming the canal, but the risk of
incarceration of the nail is high. The elastic recoil of the nail on the
endosteum at the isthmus of the shaft can make further insertion or extraction
impossible. Therefore, its unreamed use should be restricted.
Küntscher
emphasized certain prerequisites for nailing.182 Fixation must be sufficient so
that the major fracture fragments will not distract. The rigidity of the
fixation should allow for early function. Finally, whenever feasible, the
closed technique is preferred to lessen wound problems and to decrease the time
to fracture union.
Although
no experimental data have proved the optimal rigidity and strength of
intramedullary nails, clinical experience has shown that the cloverleaf,
open-slot design yields predictably good results in most cases.32,89,370 Union
rates of 98% to 99% with infection in less than 1% of cases are standard.
Midshaft fractures of the femur healed clinically and radiographically by 12 to
24 weeks after standard closed nailing.14,308,332 Shortening and malrotation
remain problems of standard Küntscher nails applied to complex fractures,370
but the overall results are as good as or better than those obtained with other
nonlocking, intramedullary nails.
Historically,
the major limitation of all nailing systems has been their poor results in
comminuted midshaft fractures and in fractures at the proximal or distal
aspects of the shaft (Fig. 27-19). The axial and rotatory loads are not
neutralized by most nails, and postoperative shortening and malrotation are
troublesome complications. Although Küntscher and others had conceived of
locking screws for such fracture patterns, widely available locking nail
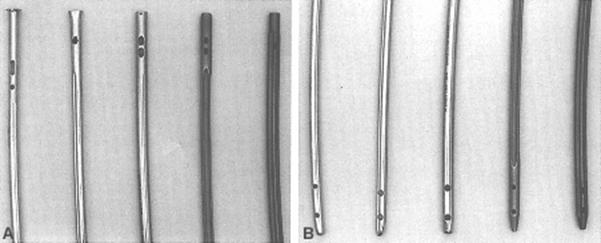
systems have been used only in the last decade. Most locking nails have a
cloverleaf cross-sectional design with one proximal hole and two distal holes
for locking of the major fracture fragments (Fig. 27-20). Transfixion screws
are inserted under radiographic control using one of a variety of techniques.
Screws in just the proximal hole or the distal holes yield a
'dynamic' fixation for fractures with potential instability in axial
compression and rotation. Static locking with screws in both proximal and
distal fragments is indicated in fractures in which both shortening and
malrotation are possible.
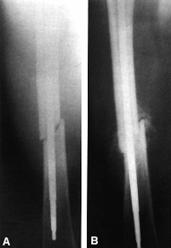
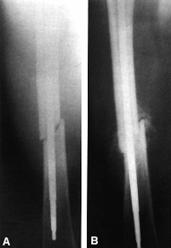
Fig. 27-19 Initial reducere
anatomica cu ulterioara telescopare si scurtare de 1,5 cm
datorita unei tije subdimensionate. Sunt specifice fracturilor oblice,
cominutive in 13 distala.
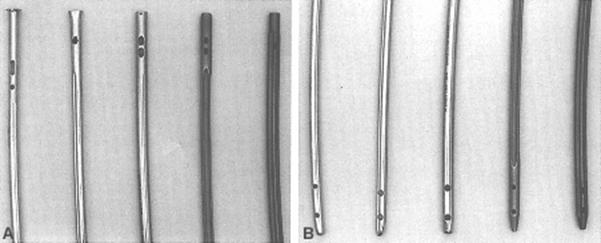
Fig. 27-20 Designul unor tije
(A-proximal; B-distal). Tije: ASIF, Grosse-Kempf, Russel-Taylor, Zimmer, Alta.
Locking
of the fracture fragments to the nail appears to have no deleterious effect on
the rapid healing that is evident after simple Küntscher nailing. Most series
of interlocking nailing report a 97% to 100% rate of union.8,88,175,176,355,372
Routine static locking of all fractures eliminates postoperative loss of
fixation secondary to unrecognized fracture comminution, which occasionally
occurs after unlocked nailing (Fig. 27-21). Various interlocking nails now form
the foundation for most intramedullary fixation systems used in North America. The clinical outcome has been found to be similar regardless of which
interlocking nail system is used. A report comparing the Grosse-Kempf,
Russell-Taylor, and Synphes interlocking nails demonstrated no difference in
the pain, limp, range of motion, or time of union of the fractures.68 Minor
design differences can influence the versatility of the various systems and the
likelihood of prominent screw heads, but all commercially available nails
appear to yield essentially comparable results.

Fig. 27-21 Fractura Winquist tip II
tratata cu tija blocata dynamic. B)Se observa, la 4
saptamani, scurtarea. Cominutia fracturii a fost
subestimata iar o tija blocata se impunea pt a preveni
aceasta complicatie
Biomechanics of
Interlocking Nailing. The optimal biomechanical conditions for fracture healing
are still unknown. Therefore, the goals of interlocking nailing of femoral
fractures are not to influence the normal cascade of fracture healing as much
as to provide a stable nail-bone construct during the healing process. This
construct should allow full loading of the bone and early functional recovery
of the limb. The biomechanical demands placed on the intramedullary nail vary
depending on fracture location and comminution, patient size, bone morphology,
and other parameters. Thus, modifications in interlocking nail design are
needed to meet these various mechanical settings.
Insertional
Properties of Intramedullary Nails. The antegrade insertion of intramedullary
nails can result in iatrogenic bursting of either the proximal or distal
fracture fragments. Several factors have been shown to predispose to this
complication.
The
average antecurvature of the femoral shaft in an adult has a radius of
curvature of about 110 cm.138 Interlocking nails are prebent to conform to this
average. If there is a mismatch in the curvatures of the femoral shaft and
nail, increased hoop stresses are generated in the femoral canal during nail
insertion. Because overreaming of the canal is performed routinely during
interlocking nailing, such mismatches are of little clinical significance
except in cases of severely abnormal femoral antecurvature.
A
second cause of increased hoop stresses and possible bursting during nail
insertion is an errant entrance portal for the nail. An anterior starting hole
in front of the pyriformis fossa results in distortion of the nail and
increased stresses within the canal.165,345,346 An excessively lateral entrance
portal can cause eccentric placement of the nail and medial comminution of the
proximal fracture fragment. The entrance portal should be located in line with
the longitudinal axis of the femoral canal in both the mediolateral and
anteroposterior planes.
The
clinical problem of iatrogenic comminution has been largely eliminated by the
routine use of overreaming and smaller-diameter, nonslotted nails.
In
Situ Properties of Interlocking Nails. Long bones are loaded in bending,
compression, and torsion. Interlocking nails are capable of restoring adequate
stiffness and strength of the fractured femoral shaft in all three of these
planes of loading.
A
fractured femur fixed with a standard intramedullary nail measuring 12 to 14 mm
in diameter is 50% to 70% as stiff as an intact femur in bending.164 This
restoration of bending stiffness occurs regardless of whether a slotted or
nonslotted nail design is used. Fractured femora fixed with static locking of
the nail fail at about four times body weight.164 Cadaveric studies have
demonstrated that when this load is exceeded, failure occurs by either proximal
screw cut-out through the trochanters or bending of the nail at the fracture
site. The Brooker-Wills interlocking nail failed at a lower load of 1.5 times
body weight by the distal fins cutting through the metaphyseal bone. The
torsional stiffness of the nail is much less than that of the intact femur,
with slotted nails being only 3% as stiff and nonslotted nails about 50% as
stiff. This torsional flexibility of interlocking nails does not result in
rotational instability of the fracture because any rotational deformation of
the femur with loading is corrected by the spring-back effect provided by
locking of the major fracture fragments.
Considerable
controversy surrounds the issue of slotted versus nonslotted interlocking
nails.95 The presence of a longitudinal slot beginning at the distal end of the
nail and extending up to or within a few centimeters of the proximal tip has
several effects on the mechanical properties of the nail. First, the slot
permits elastic impingement of the compressed nail on the endosteal surface of
the bone. Küntscher and others have postulated that this tight interference fit
with the femoral canal minimizes malrotation and shortening of the fracture.
Slotted nails also have been easier traditionally to manufacture. In addition,
the slot decreases the torsional stiffness by 15- to 20-fold compared with
nonslotted nails,344 decreases the fatigue strength of the nail,9 and decreases
the amount of metal around the locking screw holes. Thickening the nail wall of
slotted nails can lessen this problem, but also diminishes any chance of
elastic impingement of the nail on the proximal and distal fracture fragments.
Closed-section,
nonslotted nails have experienced a renewed popularity. They markedly increase
the amount of metal around the screw holes, lessening the risk of metal
fatigue. Cold working of the screw holes also has been used to strengthen the
metal around them. By varying the wall thickness, the bending stiffness of
nonslotted nails can be changed to mimic that of slotted nails, thus lessening
the risk of damage to the femur during insertion of an overly stiff nail. Such
splinting of the distal fracture fragment has been described, especially in
elderly patients in whom large-diameter nails are used.7 Change in the cross-sectional
design to a delta configuration and in the wall thickness have improved the
mechanical strength of these small-diameter, nonslotted nails (Fig. 27-22).
Such implants now are widely regarded as the interlocking nails of choice for
most femoral shaft fractures.

Fig. 27-22 Tija Russel-Taylor standard
(sus) si delta (jos)
The
necessary number of screws for distal locking has been studied for midshaft
fractures. In a cadaveric femur model, no significant difference in torsional
rigidity or axial load to failure was noted when one as opposed to two distal
screws were used.133 A parallel clinical series revealed no differences in time
to union or complication rate in cases with one versus two distal locking
screws. The judicious use of one screw probably is warranted, but a single
screw may not provide adequate stabilization of distal-third fractures. The
Brooker-Wills distal locking fins also are inadequate and provide insufficient
resistance to axial compression.20
Fatigue
Properties of Interlocking Nails. Fatigue failure through the midportion of a
standard, large-diameter (12- to 15-mm) nail or a thick-walled,
smaller-diameter nail is rare. Deformation and breakage is more common at the
proximal or distal ends of interlocking nails. Several factors may predispose
to failure at these locations. First, overreaming of the medullary canal and
the use of undersized interlocking nails leads to little contact of the nail on
the endosteum and concentration of loading at the proximal and distal screw
sites. The holes in the nails decrease the amount of metal and the strength of
the nail to an appreciable degree. Most manufacturers now thicken the nail
wall, widen the proximal nail diameter, or cold work the holes to enhance the
nail fatigue life at these sites. Despite these improvements, fatigue failure
can occur if fracture healing is delayed or early excessive loading is
permitted.
The
most common site for fatigue failure is at the most proximal of the two distal
locking holes for most interlocking nails (Fig. 27-23). Finite element analysis
of interlocking nails has revealed that if a fracture is located within 5 cm of
this hole, stresses are generated in the nail above its endurance limit63 (Fig.
27-24). Once fracture healing has proceeded sufficiently to restore 50% of the
normal stiffness of the distal femur, the stresses are diminished below that of
the endurance limit of the nail. Improvements in nail design, such as
nonslotted cross sections, cold working of the holes, and thicker nail walls,
have lessened the prevalence of nail fatigue at this level. Nevertheless,
infraisthmal fractures stabilized with interlocking nailing should be managed
with delayed weight bearing until bridging callus is evident on radiography.
Another
weak area of certain interlocking nails is at the proximal weld between the
cylindrical and slotted portions of the nail. In one study, prototypical nails
were welded at this junction, and fatigue failure was common when the nails
were used for high subtrochanteric fractures and cases of nonunion.113 The
manufacturing process of partially slotted nails has been changed, and proximal
welds no longer are present in most nail systems. Implant failure in cases of
delayed union of proximal-third fractures now involves mainly screw breakage.
SPECIAL SITUATIONS
Simple
transverse and short oblique midshaft fractures without associated fractures or
soft-tissue injuries are managed readily by closed interlocking nailing. Many
fractures of the femoral shaft, however, are more complex in their fracture
anatomy, location, or associated injuries. Therefore, most shaft fractures
necessitate some modification of the standard nailing technique. The following
common situations alter the specific preferred treatment of shaft fractures.
Comminution
Comminution is a
sign of a high-energy injury. Comminuted fractures are associated with a
greater blood loss into the thigh and, frequently, with open-fracture wounds.
The prevalence of systemic complications, such as fat embolism, also is higher.
The Winquist classification of comminution is based on the degree of
circumferential fragmentation of the shaft369,370 (see Fig. 27-6). It was
designed to evaluate the feasibility of achieving a stable surgical construct
with intramedullary fixation. Nondisplaced comminution of the proximal or
distal fragments may not be apparent on the diagnostic radiographs, and only
become manifest during the intraoperative or postoperative period.59
The
presence of fracture comminution traditionally has complicated the decision
making on preferred treatment. Simple cloverleaf nails have been found to be
contraindicated for type III and type IV comminuted fractures because of the
risk of shortening of the fracture around the nail. Small-diameter nails fail
to fill the canal, allowing even type I and type II comminuted fractures to telescope
around the nail. Before the advent of interlocking nails, standard cloverleaf
nails supplemented with cerclage wiring of major cortical fragments were widely
used for comminuted fractures (Fig. 27-25). This method requires wide exposure
with a system of wire passage and wire tightening. A minimum of two wires are
used for each major fragment, the soft-tissue attachments of which should not
be disturbed. A variety of materials have been recommended for cerclage.
Stainless steel, 16- or 18-gauge wire results in negligible disruption of the
periosteal blood flow and little necrosis of the underlying bone. Parham bands,
with their wider diameters, are easy to use and effectively stabilize cortical
fragments of variable sizes.263 However, they interrupt blood flow over a 1-cm
length of bone and should not be used.
The
slow healing observed after open intramedullary nailing and cerclage also can
be attributed to the disruption of the fracture hematoma. Removal of the
scaffolding of the fracture hematoma with its complement of cytokines and
growth factors lessens the initial inflammatory and subsequent proliferative
stages of fracture healing. Combined with the surgical devascularization of the
cortex, this violation of the fracture hematoma invariably has a measurable,
deleterious effect on the speed of fracture healing.
The
clinical results with cerclage wiring are satisfactory but clearly inferior to
those of closed static interlocking nailing.378 The early Seattle experience
with 245 comminuted fractures revealed an infection and nonunion rate of less
than 1% and a shortening and malunion rate of only 5%.370 The good results were
attributed to routine delay of weight bearing until advanced healing of the
fracture was evident on radiography.
Interlocking
nails have supplanted other therapies for comminuted fractures. These nails
fill the medullary canal of the proximal and distal fragments, thereby
restoring femoral alignment. Reduction of the comminuted fragments is
unnecessary because abundant callus engulfs them (Fig. 27-26 and Fig. 27-27).
Serial radiographs usually demonstrate progressive lessening of the angulation
and translation of displaced cortical fragments as fracture healing proceeds.
Such consolidation of these fragments is due to the hydrostatic effect of the
surrounding muscles and the organization of the fracture callus. Persistent
displacement of butterfly fragments has no deleterious effect on function
except for the rare situation in which the fragment is buttonholed into the
quadriceps muscle or through the iliotibial band. Fragments displaced more than
2 cm from the medullary canal do not contribute to the healing fracture and are
not incorporated in the fracture callus.86 Static locking of the major fracture
fragments prevents postoperative shortening and malrotation of the fracture.
The high prevalence of unexpected comminution has led many authors to recommend
routine static locking of all femoral shaft fractures.59 The published results
with interlocking nails are superior to those of other treatments.163,349,378
Wiss and coworkers372 reported a 98% union rate without any infection in a
large series of comminuted and rotationally unstable fractures.
A
specific variant of comminuted fractures, the segmental fracture, involves a
double-level fracture of the shaft. The proximal fracture may approach the
subtrochanteric region, and the distal fragment may approach the supracondylar
region of the bone. As high-energy fractures, the individual fractures may be
comminuted and each fracture must be assessed for its degree of instability.
The good results achieved with closed interlocking nailing eclipse those
attainable with other therapies for segmental fractures.368,378 Although
technically demanding, the closed technique usually is applicable and yields
predictably good results.
Proximal and Distal Fractures
When the
fracture is a distance proximal or distal to the isthmus of the medullary
canal, the feasibility of achieving stable fixation with a conventional
intramedullary nail diminishes. Failure of the nail to fill the canal of either
the proximal or distal major fragment, especially for fractures at the junction
of the metaphysis and diaphysis, leads to postoperative instability in both
axial compression and rotation. Fracture angulation also is possible during
surgery if the nail is driven eccentrically out of alignment with the
longitudinal axis of the canal. Such operative malalignment is especially a
problem with distal fractures in which the nail is driven into the medial or
lateral condyles, resulting in either a valgus or varus deformity,
respectively. The mechanical demands on the nail also are increased.
Subtrochanteric and high proximal-third fractures are subjected to major
muscular forces and high concentrations of tensile forces along the lateral
cortex.310 Supracondylar fractures have similar load concentrations in both the
sagittal and frontal planes.
High
Proximal-Third and Subtrochanteric Fractures. High
proximal-third and subtrochanteric fractures encompass a wide spectrum of
proximal femoral fractures, and the distinction between these two areas often
is blurred. The biomechanical stresses of this area historically have led to
separation of these injuries from pure femoral shaft fractures, because the
rates of nonunion and hardware failure are higher in this region than in any
other in the femur.310 The anatomical relationships of the fracture lines and
the continuity of the proximal femoral fracture fragment must be understood to
conceptualize the appropriate therapy for an individual injury within this
region.
Classification
of these fractures has undergone refinement through the years. Simplistic and
outdated classifications, like that of Fielding and Magliato,111 were based
merely on the distance below the lesser trochanter. The Seinsheimer
classification,317 which is widely quoted, and the AO classification239 use the
details of the obliquity of fracture lines and the degree of comminution of the
medial femoral cortex to differentiate between their fracture types. Although
these classifications helped orthopaedists understand that fractures with
medial comminution have higher rates of varus collapse and failure of fixation,
their usefulness was related to proximal femoral fractures treated with open
reduction and plating. With closed interlocking techniques, the specifics of
the fracture pattern below the lesser trochanter has little or no bearing on
the treatment, diminishing the applicability of these accepted classification
schemes. For conceptual purposes, fractures of the proximal third of the femur
can be widely differentiated into those with the proximal fragment intact to a
level below the lesser trochanter, those with the proximal fragment intact but
with dissociation of the lesser trochanter, and those subtrochanteric fractures
with proximal extension into the intertrochanteric region.
Proximal-third
fractures usually are high-energy injuries of young adults. In this patient
population, the proximal femoral fragment generally is intact to a level below
the lesser trochanter, creating a true subtrochanteric fracture, often with
distal extension into the femoral isthmus and beyond. In older patients,
proximal extension into the greater trochanter and intertrochanteric region is
more common. Because the method of fracture stabilization depends on the
integrity of the proximal fragment, the clinician should look specifically for
fractures involving the greater or lesser trochanter in the radiographic
assessment. Fracture extension into one or both of these areas often precludes
the use of conventional intramedullary nails. Multiple radiographic views may
be necessary to demonstrate longitudinal fracture lines that can displace
during nail insertion and preclude adequate interlocking fixation.
Treatment
decisions can be difficult with this spectrum of injuries. Nonoperative methods
of traction and cast bracing are poor choices for proximal femoral fractures
because they inadequately counteract the deforming muscular forces around the
hip. Because this area is prone to varus collapse, patients who are permitted
to ambulate before fracture consolidation have unacceptably high rates of varus
malunion. Condylocephalic rods, such as Ender rods, have been used for
proximal-third femoral fractures, but their poor mechanical properties and
questionable stability restrict their usefulness. Their insertion is
technically difficult, and postoperative bracing or continued traction often is
required to maintain alignment. For these reasons, these devices have fallen
out of favor for the fixation of proximal femoral fractures.144
Open
reduction with plating has been advocated by many investigators. The 95°
condylar screw or blade plate (Fig. 27-28) has the advantage of providing
excellent purchase on the proximal fragment.30,96,173,174,224,245 These designs
obtain multiple screw fixation of the head and neck fragment as opposed to the
standard 135° or 150° compression hip screw devices. The barrel of the hip
screw devices often enters the fracture site, and this device usually gains proximal
fragment fixation only with the proximal large lag screw. Although advances in
metallurgy have increased the strength of the sliding hip screw designs,
rotational control of the proximal fragment is lacking because of this single
screw purchase. Therefore, unlike intertrochanteric fractures, the 95° devices
unquestionably provide better fixation than do the more familiar hip screws for
proximal-third femoral fractures.96 However, good results have been obtained
with either device when reconstruction of the medial buttress of the proximal
femur has been obtained.186,238,320
The
technique of open reduction has changed substantially over the past decade.
Once, rigid internal fixation with anatomical restoration of the fracture
anatomy was desired. Although this gained superior stability, it created the
need for increased dissection of the fracture, rendering more of the fragments
avascular. Bone grafting was recommended in most of these procedures,
especially if the medial wall was comminuted, as a stimulant to fracture
healing. Recently, the so-called 'indirect' reduction methods have
been popularized.174 These techniques sacrifice anatomic restoration of the
fracture fragments to ensure their viability. The medial soft tissues and
fragments are left relatively undisturbed, permitting fracture healing through
natural external callus. Bone grafting, and the need to dissect medially for
its placement, usually are unnecessary with these techniques. Because of the
decrease in iatrogenic damage within the zone of injury, these methods
theoretically can produce a higher rate of fracture healing with a decrease in
the prevalence of infection and hardware failure. Good comparative studies of
these two techniques (extensive open reduction and rigid fixation vs. indirect
reduction and fixation) are not available224; however, a decrease in these
complications has been reported.174 Further study is necessary to determine
whether plating by indirect reduction methods for subtrochanteric fractures
provides a safeguard against the complications that are inherent with any
plating of the femur.353
The
Zickel nail was designed for subtrochanteric and high proximal-third shaft
fractures. It is a rigid, short, noncannulated, prebent nail through which a
triflanged nail is inserted into the femoral head and neck.382 Accurate
placement of the nail can be difficult, especially in patients with anatomic
variations of the proximal femur and in those with comminution of the greater
trochanter. Nevertheless, its design decreased the biomechanical lever arm
inherent in this area, and good results have been reported.27 However, its
design did not permit axial or rotational control of the distal fragment, and,
although insertion by closed technique has been reported,281,305 open reduction
and cerclage wiring of the fracture routinely is required to obtain
stability.280 Furthermore, a major complication of the device occurred with
nail extraction, where a disturbingly high rate of refracture of the femur was
noted, often at a level different from that of the original fracture.255
Because of this complication, the Zickel nail is contraindicated in young
patients and should be considered only for older patients or those with
pathologic fractures. This device represented a great advance in the late
1970s, but it has largely been replaced by other intramedullary designs and is
implanted only rarely today.
Interlocking
intramedullary nailing is the treatment of choice for subtrochanteric fractures
and fractures of the proximal third of the femur in which the lesser trochanter
is in continuity with the proximal fragment.5,45,259,371,380 The oblique
interlocking screw obtains excellent purchase on the medial cortex, usually
just anterior to the lesser trochanter, providing excellent stabilization of
the proximal fragment (Fig. 27-29). Interlocking nails available today are much
stronger than early designs and are less susceptible to device deformation and
failure in spite of the large biomechanical stresses of this region.220 A
correct starting portal in the piriformis fossa is mandatory, because placement
too lateral in the greater trochanter will shift the proximal fragment into
varus malalignment and will drive the nail into the medial femoral cortex,
possibly increasing fracture comminution. Many investigations have demonstrated
the superiority of the interlocking nail over open plating and the Zickel nail
in the treatment of subtrochanteric fractures.45,245,320,371 With closed
interlocking nailing, the biomechanical stresses of the subtrochanteric region
no longer threaten the security of the fixation, and the results of these
fractures approach those seen with midshaft femoral injuries. Once grouped as a
separate and more complex injury than midshaft fractures, subtrochanteric
fractures with the proximal fragment intact to a level below the lesser
trochanter no longer exhibit such clinical difficulty. Plating of femoral
fractures with an intact proximal fragment to a level below the lesser
trochanter generally should be considered a choice of treatment second to
interlocking nailing.353
The Gamma nail, a short
intramedullary hip screw,205,322 has been advocated for intertrochanteric and
subtrochanteric fractures of the femur. The published results of this device
vary widely,36,120,197 and its applicability to subtrochanteric fractures
remains controversial. Because of the relatively high rates of refracture of
the femoral shaft below the tip of the implant reported in large studies of hip
fractures,204,274,365 this device cannot be recommended for subtrochanteric
fractures.
For
subtrochanteric fractures in which the lesser trochanter is dissociated from
the proximal fragment but the remainder of the proximal femur remains intact,
interlocking nails with the standard oblique interlocking screw are unable to
provide fixation. Interlocking nails with the proximal screws directed into the
neck and head of the femur are required (Fig. 27-30 and Fig. 27-31). Because of
the complexity of this surgery, patient numbers in published series using this
technique are relatively small compared with the large patient populations in
investigations using standard interlocking techniques. Nevertheless, for this
injury, the results of these studies have been promising, despite an increase
in the technical difficulty of nail insertion.37,169,327 Because the piriformis
fossa lies posterior to the femoral neck, anteversion is built into these
devices to ease correct placement of these proximal interlocking screws. If the
proximal fragment has fracture extension into the area of nail insertion, then
the nail can displace posteriorly through the fracture site. Fractures into the
piriformis fossa, therefore, are relative contraindications to intramedullary
nailing and open reduction with plating should be considered. Further discussion
regarding these difficult intertrochanteric/subtrochanteric fractures is found
in Chapter 26.

Fig.
27-31Tija de reconstructie Russel-Taylor
Supracondylar
Fractures. Infraisthmal and supracondylar fractures
pose problems similar to those of proximal fractures. Infraisthmal fractures,
defined as fractures extending from the isthmus of the medullary canal to the
supracondylar region, include most distal-third shaft fractures. These
fractures are notorious for a high complication rate after plating and screw
fixation, especially when rigid fixation is not achieved.336 The major loading
of this region of the femur, along with the inadequacy of endosteal purchase on
the distal fragment, also results in a higher nonunion rate with interlocking
nails than is seen in midshaft fractures. Despite these obvious mechanical
limitations, the results with interlocking nails are superior to those of
closed treatment and those of plating.286
Supracondylar
fractures present additional mechanical and technical problems. Traction and
cast bracing are hampered by a tendency toward varus and internal rotational
deformity. Malunion is common.286 Good results are attainable with the 95°
angled blade plate or screw plate if there is close adherence to the ASIF principles
of rigid fixation. Placement of the blade plate in all three planes must be
precise. Double plating (lateral and medial) is indicated in unstable fractures
with extensive medial comminution.304 Bone grafting and delayed weight bearing
normally are required as part of the postoperative regimen. The indirect
reduction technique with minimal exposure of any comminuted fragments can be
especially useful in the AO type A3 and C3 injuries.33
A
major complication of plating of distal-third shaft fractures is refracture
after removal of the plate. Refracture is especially likely if supplemental
interfragmental lag screws were used for the initial internal fixation.38
Cortical atrophy under the plate and the stress riser effect of the screw holes
combine to result in refracture with minor trauma in nearly 10% of cases in
which plates are removed, regardless of the timing of plate removal. Refracture
can be treated easily by closed intramedullary nailing.
The
Zickel supracondylar device was designed specifically for the problem of
comminuted distal fractures in osteoporotic bone.383,384 The flexible,
sled-shaped ends of the Zickel nails are inserted through the medial and
lateral condyles up into the medullary canal. The ends are tapered for ease of
insertion, and closed insertion under fluoroscopic control is feasible in most
cases. The nails are anchored to the condyles with screws. Although a high
union rate is obtained with these implants, shortening of the fracture around
the nails does occur. Because of its poor mechanical properties, use of the
Zickel supracondylar device should be limited to low supracondylar fractures in
the elderly.
A
cannulated, prebent interlocking nail called the GSH (Green, Seligson, Henry)
supracondylar nail has been designed specifically for low infraisthmal and
supracondylar fractures200 (Fig. 27-32). It is inserted in a retrograde fashion
through an entrance portal in the intercondylar notch of the distal femur. When
the nail is inserted using a closed technique, rapid fracture healing can be
expected. Severe osteopenia of the distal femur may necessitate supplemental
external fixation with a cast brace. Nail breakage remains a problem and
modifications in the nail design, including larger-diameter nails, small
locking holes, and a nonfenestrated central portion to the nail, have been
recommended.155 The exact role of this nail in the management of AO type A and
type C supracondylar/intercondylar fractures will not be clear until larger
clinical studies are available.200
Interlocking
nails with distal screw fixation yield excellent results for most distal
fractures (Fig. 27-33). They are the preferred implant for most infraisthmal
fractures and for selected supracondylar fractures. Two distal locking screws
are needed to ensure sagittal plane stability. The risk of implant failure
through the most proximal of the distal screw holes mandates delayed weight
bearing until fracture healing has progressed.63 The Brooker-Wills nail with
locking fins in place of distal locking screws has been used extensively for
these distal-third shaft fractures.47 However, technical problems with
insertion limit the usefulness of this nail for distal-third fractures as well
as for any shaft fractures.23 A more detailed description of supracondylar fractures
is provided in Chapter 30.
Open Fractures
Open fractures
of the femoral shaft often result from high-energy accidents and frequently are
accompanied by injuries to multiple organ systems.15,74,76 Open fractures of
the femur traditionally have been treated with debridement and skeletal
traction. Clinical research in the last several decades has demonstrated that
several major benefits can be derived from a more aggressive surgical approach.
Retrospective
studies in the 1970s and 1980s demonstrated that the multiply injured patient's
chance of survival was increased by immediate fixation of long-bone
fractures.122,163,218,288,289,314 A randomized prospective study by Bone and
colleagues34 showed that immediate stabilization of femoral shaft fractures in
the multiply injured patient resulted in a decreased prevalence of adult
respiratory distress syndrome, fewer days in the intensive care unit, and
decreased hospital costs. These investigations heightened the awareness of
orthopaedists and trauma surgeons to the importance of early orthopaedic
intervention in their patient populations.
The
introduction of interlocking nailing widened the spectrum of femoral shaft
injuries that could be stabilized by closed intramedullary techniques. Open
fractures often are characterized by severe fracture comminution, bone loss,
and a proximal or distal fracture level. Interlocking nails are uniquely suited
to handle these fracture patterns, and the results of interlocking nailing have
been superior to those of all other previous treatment methods.162,372
Finally,
dissatisfaction existed with the accepted treatment alternatives. Skeletal
traction, which permitted little patient mobility, did not allow adequate wound
access and was associated with high rates of pulmonary complications in the
multiply injured patient.34,288 This method provided the least softtissue and
bony stability of all treatment options, factors thought to be important in the
control of infection in open fractures.75,76
Intramedullary
nailing by open technique,167,199 open nailing with cerclage wiring,163,351 and
open reduction and plating of open femoral shaft fractures18,124,203,290,300
resulted in unacceptable rates of infection, and these techniques were readily
abandoned for these injuries. The high rates of infection were attributed to
the cumulative effects of bone and tissue necrosis resulting from the injury,
contamination introduced at the time of the accident, and further tissue
devitalization during surgical dissection.
The
closed insertion of multiple nonreamed intramedullary rods, such as Ender
rods,121,207,237,257 theoretically provides an attractive alternative to open
reduction, because nonreamed intramedullary nailing disrupts the endosteal
vascular supply to a lesser degree than does reamed intramedullary nailing.284
The frequent complications of knee pain, unstable fixation, and malrotation,
however, have diminished the popularity of this technique.52,106,144
External
fixation provides excellent bony stabilization, wound access, and early patient
mobilization, avoiding most disadvantages of skeletal traction. Unfortunately,
in a substantial percentage of open femoral fractures treated with external
fixation, decreased range of motion of the knee and pin-tract infection
develop, leading to suboptimal results.132,241 However, the prevalence of
chronic infection at the fracture site is markedly decreased in injuries
treated with this technique, as compared with previously discussed
methods.18,21,294,295,358
Before
the 1980s, closed intramedullary nailing was not commonly performed in open
femoral fractures.57,77,194 Theoretic reasons to avoid its use include the
following: (1) all open fractures are contaminated injuries; (2) all open
fractures have some degree of tissue crush, necrosis, and periosteal stripping;
and (3) reaming the medullary canal devascularizes the bone further through
obliteration of the endosteal blood supply.3,251,284
Chapman76
suggested that open femoral fractures be treated with delayed intramedullary
nailing, usually 5 to 7 days after wound closure. This delay allowed the immune
system to control existing fracture-site contamination, decreasing the rate of
postoperative infection. He reported no infections with delayed closed
intramedullary nailing of grade I and grade II open fractures, which were
stabilized initially with skeletal traction.76 Despite these excellent results,
delayed nailing failed to provide the benefits of early fracture fixation in
the multiply injured patient.
Winquist
and colleagues370 performed immediate and delayed closed intramedullary nailing
in open femoral shaft fractures after wound debridement and found it to be a
safe technique in grade I and grade II open injuries. They recommended
immediate stabilization of these less severe open fractures, because the
prevalence of infection (2%) was not affected by the timing of the operative
stabilization. These findings have been substantiated by the later
investigations of Lhowe and Hansen,194 Brumback and colleagues,57 and
others.128,248 Each investigator emphasized the requirement of a thorough wound
debridement before intramedullary nailing and stressed the selection of
appropriate candidates for the procedure (Fig. 27-34).
Two
major considerations must be evaluated in deciding whether an open femoral
fracture is best treated by immediate intramedullary nailing. First, multiply
injured patients with an ISS greater than 18 run a high risk of pulmonary
complications and benefit from early fracture stabilization on the day of
injury.
Second,
the size and contamination of the soft-tissue wound must be accurately
assessed. The Gustilo classification of open fractures,130,131 which is used
most commonly in assessing soft-tissue injury, defines three specific variables
in determining the applicability of intramedullary nailing to a given open
fracture: the time after injury; the degree of tissue necrosis, crush, and
periosteal stripping; and the magnitude of the wound contamination.
Because
all open fracture wounds are contaminated, and the bacterial flora continues to
proliferate over time, the time since injury may be an important factor in the
development of wound infection. The longer the contamination remains unchecked,
the greater is the risk of infection.292 This is reflected in the Gustilo
classification by the categorization of any open fracture in which debridement
is delayed more than 8 hours as a grade III open fracture. Brumback and
colleagues57 suggested that immediate intramedullary nailing of open femoral
fractures was contraindicated if the debridement procedure was performed more
than 8 hours after injury. Therefore, a timely, thorough debridement is a
prerequisite to immediate intramedullary nailing. With severe soft-tissue
injury, the response of the tissues to the bacterial contamination is
compromised. Therefore, wounds with minimal tissue crush and periosteal
stripping (Gustilo grade I and grade II injuries) carry a lower risk of
infection after immediate intramedullary nailing than do those with severe
soft-tissue injuries.
Injuries
accompanied by extreme contamination, such as farm accidents, shotgun blasts,
and explosions, are considered grade IIIB open fractures and have high rates of
infection, regardless of the method of fracture fixation.76 The risk of
infection undoubtedly is increased if the contamination occurs in a severely
injured soft-tissue environment. The presence of gross contamination in the
medullary canal of the major fracture fragments should preclude immediate
internal fixation.
Taking
all these factors into account, the following treatment guidelines have been
developed. A systemic antibiotic, usually a cephalosporin, is administered, and
the patient is prepared for surgery after emergency resuscitation and
assessment. Before any external or internal fixation is undertaken, all open
wounds are debrided radically and the degree of contamination of the fracture
site is assessed. Jet lavage irrigation with a minimum of 6 to 10 L of fluid is
used during debridement. Surgical wounds can be closed, but all traumatic
wounds are packed open. Regardless of the magnitude of the multiple organ
system injury, grade I and grade II open fractures without gross medullary
contamination are treated best by immediate intramedullary nailing. The
multiply injured patient with an open femoral fracture should be treated with
some form of immediate stabilization; a patient with a grade IIIA open femoral
fracture can be treated safely with immediate intramedullary nailing, if the
debridement is performed within 8 hours of injury. If the debridement is
delayed or if a grade IIIB injury is present, then external fixation may be the
treatment of choice. No investigation has studied the delayed conversion of
external fixation to intramedullary nailing with respect to open femoral fractures.
In patients without multiple injuries, grade IIIA and selected grade IIIB open
femoral shaft fractures can be placed in temporary skeletal traction, awaiting
wound closure. Delayed intramedullary nailing is performed 5 to 7 days after
soft-tissue coverage. Isolated open fractures with severe contamination require
external fixation.
For
those fractures associated with arterial lesions (grade IIIC) that require
repair, external fixation may be the best method of immediate stabilization
because it can be applied quickly and then realigned after vascular repair.
After revascularization of the limb, this fixation can be converted to an open
plating or an intramedullary nailing, even on the day of injury. Plating of
grade IIIC open fractures has been suggested because the surgical exposure to
the bony injury usually is already performed for the vascular repair.193 A
grade IIIC open fracture in an unstable multiply injured patient may be a
relative indication for limb ablation, because the critical nature of the
patient's condition and other organ system injuries can make limb
revascularization a life-threatening procedure.
When
intramedullary nailing is selected as the method of stabilization, it should be
performed as a separate operative procedure after wound debridement.57 The
nailing is performed through a standard antegrade approach on a fracture table.
High rates of fracture union are reported in open femoral fractures treated in
accordance with these guidelines. Bone grafting usually is not necessary despite
the loss of small devitalized cortical fragments from the injury and
debridement.57 Chapman73 has shown closed intramedullary bone grafting to be an
excellent technique for segmental bone loss of the femoral shaft. Such surgery
is most effective if it is performed several weeks after soft-tissue coverage
is achieved.
Reports
in the literature indicate low rates of infection for grade I, grade II, and
grade IIIA injuries treated in accordance with these guidelines, but most
authors agree that grade IIIB injuries remain a therapeutic problem.57,194 No
large series of grade IIIC open femoral shaft fractures exists, but the
reported cases document the relatively poor limb function and high prevalence
of late infection in these injuries.104
Nonreamed
interlocking nails are being investigated for open femoral fractures. These
devices represent a potential advance in the treatment of open femoral shaft
fractures because the bone necrosis created by medullary reaming may be
diminished. No long-term data on the results with these implants are available.
Concern over the durability of these smaller implants has been expressed, yet
the early clinical experience has been favorable. Recent concern over reamed
intramedullary nail insertion having a potential deleterious effect on
pulmonary function has led to an increase in the use of nonreamed nails for
both open and closed femoral fractures. Further study is required in this area.
Ipsilateral Femoral Neck and Shaft Fractures
Concurrent
ipsilateral femoral neck fractures are reported in 2.5% to 5% of patients with
femoral shaft fractures.17,71,114,339,340,373 The wide variability of fracture
patterns of the proximal femur and shaft challenges the treating orthopaedist.
Since the first description of this complex injury by Delaney and Street in
1953,101 more than 70 methods of treatment have been reported in hundreds of
cases.340 There has been a recent resurgence of interest in these injuries.26,
37, 81, 189, 262, 278, 373, 376, 377 Some investigations include only those
injuries with ipsilateral femoral neck and shaft fractures,37,141,148,339,373
whereas others expand the category of proximal injuries to include
intertrochanteric fractures.17,29,71,114,117 In all published series, femoral
neck fractures occur more often in conjunction with femoral shaft fractures
than do intertrochanteric injuries, by a ratio of about 7:1.26 Reflecting the
high-energy nature of these injuries, associated knee injuries, including
patellar fractures, tibial plateau fractures, and intraarticular injuries,
often accompany the femoral fractures.26
Whereas
the shaft fractures vary widely in their location and comminution, the neck
fractures usually are a vertical shear (Pauwels grade III) pattern373 (Fig.
27-35). The typical neck fracture commences inferiorly at the base of the
femoral neck and travels superiorly to the subcapital portion of the neck.
Because much of the impact energy of the injury is dissipated at the shaft
fracture, the neck fracture usually is minimally displaced and noncomminuted.
Therefore, the prevalence of osteonecrosis of the femoral head is low after
this combined femoral fracture.26
Diagnosis
of the neck fracture often is delayed because of failure to evaluate the entire
femur radiographically when there is a shaft fracture.26,278 About one fourth
to one third of neck fractures initially are overlooked, and then subsequently
are detected after stabilization of the shaft fracture.26,278 Some do not
become apparent until weeks after the patient has been discharged from the
hospital.278 Delayed diagnosis is not associated with an increased rate of
femoral head osteonecrosis26 and most cases can be salvaged with good
functional results by closed reduction and insertion of multiple pins or screws
around in situ nails.
The
literature describes some of the femoral neck fractures as iatrogenic injuries
created at the time of intramedullary nailing.138,140 It is difficult to
separate this group from those that are present before surgery but are
recognized only after the procedure. Although an incorrect starting position of
the intramedullary nail may increase the likelihood of an iatrogenic neck
fracture, it is probable that many of these injuries are not recognized before
surgery and then are attributed to, or propagated by, the surgical procedure.
Plain radiographs of the proximal femur, preferably with 15° internal rotation
of the hip, should be obtained as part of the initial evaluation followed by
fluoroscopic evaluation of the hip once the patient is positioned for the
nailing procedure.
Femoral
neck nonunion and malunion are more common problems than are osteonecrosis of
the femoral head26,37,373 or complications secondary to the shaft fracture.
Therefore, it is important to give priority to anatomical reduction and rigid
internal fixation of the femoral neck fracture.81 Subcapital and transcervical
fractures usually are stabilized with lag screws; fractures occurring at the
base of the neck or the intertrochanteric region can be treated best with
sliding compression screw devices. The former fixation is compatible with a
wide range of treatment options for the femoral shaft, whereas the latter
greatly restricts the alternatives for femoral shaft fixation. The historical
dilemma in the treatment of these injuries is thus demonstrated: to obtain
anatomical reduction and rigid fixation of the neck fracture without
compromising the treatment of the femoral shaft fracture.
Anatomical
reduction of the femoral neck usually can be achieved even in the presence of
an unstable shaft fracture. Malreduction of the neck fracture results in
nonunion in many patients.26,37 Symptomatic varus nonunion has been reported to
occur in as many as 18% of these injuries and requires proximal femoral valgus
osteotomy to achieve union.373 Fixation of the femoral neck fracture ideally
should provide compression across the fracture site. Therefore, devices such as
the Ender rod, the Zickel nail,17 and the Williams nail143,150 are poor choices
for fixation, despite having been used successfully in the past. These implants
tend to distract the femoral neck fracture, possibly increasing the prevalence
of nonunion. If rigid, intrafragmental compression of the neck fracture is
accomplished, fracture healing within 3 to 6 months can be expected with most fixation
techniques.
The
most commonly reported method of fixation is antegrade intramedullary nailing
of the femoral shaft fracture combined with multiple pin or screw fixation of
the femoral neck fracture.26,189,373 An alternative retrograde technique with
insertion of a short nail through the side of the medial femoral condyle has
been proposed to allow for more space for accurate insertion of the femoral
neck screws.340 However, interlocking nails cannot be readily inserted with
this method, compromising fixation in comminuted, oblique, or spiral femoral
shaft fractures. Although excellent results have been reported with this
retrograde nailing protocol, it has not received widespread acceptance. A
different retrograde technique using an intraarticular, intercondylar entrance
portal permits the use of standard interlocking nails but remains experimental
at this time228 (see Fig. 27-36). Both these retrograde methods must be used
cautiously because retrograde nailing imparts a cephalad load in the proximal
femur that can lead to varus displacement of a femoral neck fracture.
Antegrade
nailing and screw fixation of an ipsilateral femoral neck and shaft fracture
are technically demanding.373 Accurate placement of three or four 6.5-mm
cancellous screws is important to prevent obstruction of the intramedullary
reamers or passage of the nail (Fig. 27-37). The use of cannulated lag screws
assists in precise screw insertion anterior to the nail and centrally in the
head and neck of the femur.189 Placement of at least one screw before
intramedullary nailing is suggested to prevent displacement of the femoral neck
fracture.62 The major complication of this technique has been failure to
achieve anatomical reduction of the femoral neck fracture. If the neck fracture
is markedly displaced or irreducible, an anterior open reduction with
provisional K-wire or screw fixation of the neck should be performed.
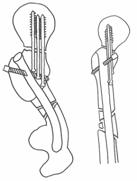
Fig. 27-37 Relatia corecta
dintre suruburile de col si tija. De remarcat punctul de intrare
anterior si traiectul spre cortexul posterior al capului femoral.
Although
interlocking nailing improved the treatment of the shaft fracture, it was not
until the introduction of the second-generation interlocking nails, such as the
femoral reconstruction nail, that closed intramedullary fixation could securely
stabilize both the proximal and shaft fractures with a single device. The
proximal end of the nail is designed to accommodate two smooth-shanked lag
screws that gain purchase in the head and neck of the femur (Fig. 27-38). These
screws serve both to fix the neck fracture and to lock the shaft fracture.
Anteversion of these two screws of about 10° has been designed into these nails
to allow passage of the lag screws through the nail and up the femoral neck.
Biomechanical
studies of cadaveric femora demonstrate that the ultimate strength of the
reconstruction nail fixation of the neck fracture is higher than that afforded
by cancellous screw fixation alone.275 The passage of the locking screws
through the nail prevents varus collapse of the neck fragment, which is seen
often when only cancellous screws are used. The bending moment on the proximal
screws also is decreased by their passage through the nail. Therefore, the mode
of failure after fixation of an ipsilateral neck fracture with a reconstruction
nail is more likely to be cutting out of the locking screws.275
Because
of the requirement for accurate placement of the proximal screws in the
second-generation interlocking nails, these devices are even more technically
demanding than is routine interlocking fixation.373 The femoral canal should be
overreamed 1.5 to 2 mm larger than the nail to allow for adjustment of the
anteversion angle. Because the neck originates anteriorly on the proximal
femur, the nail often must be externally rotated 30° to 40° to obtain a
bulls-eye screw placement in the femoral head. This may be true even with the
built-in anteversion in these nails. If the nail is not driven in a proper
distance, only one screw can be inserted into the head and neck.37 The lateral
alignment of the proximal screws can be observed on fluoroscopy by the proximal
targeting jig. It is critical, therefore, that careful attention be paid to the
depth of nail insertion and its rotation in the femur. If inaccurate alignment
is noted, the nail should be removed and repositioned, and the alignment of the
guide pins for the locking screws should be rechecked. Several series of neck
and shaft fractures stabilized with reconstruction nails have reported
satisfactory results.
Femoral
shaft fractures also are associated occasionally with hip dislocations,
acetabular fractures, or pelvic ring disruptions189,376 (Fig. 27-39).
Functional results are optimized by early rigid fixation of all fractures.
Emergency reduction of hip dislocations, often with the assistance of a
temporary external fixation pin in the proximal femur, is mandatory. If
extensile exposure and dissection of the gluteal musculature is necessary for
acetabular or pelvic ring fractures, heterotopic ossification between the
pelvis and the trochanteric entrance portal of the femoral nail is a serious
problem. Prophylactic radiation therapy or indomethacin therapy helps lessen
the prevalence of heterotopic ossification in such cases.
Ipsilateral Femoral Shaft and Intercondylar Fractures
An intercondylar
fracture of the distal femur rarely accompanies a fracture of the femoral
shaft. When the combination does occur, two distinct types can be identified:
(1) the intercondylar fracture that does not propagate proximally to be
contiguous with the shaft fracture, and (2) the intercondylar fracture that
forms a distal extension of the shaft fracture.
These
injuries traditionally have been treated by a variety of techniques, including
open reduction of both fractures with a single plate, open reduction of both
fractures with two separate plates, and open reduction of the intercondylar
fracture and intramedullary nailing of the femoral shaft injury. Interlocking
nailing has provided the ideal opportunity to combine the stabilization of
these two injuries, especially in cases of nondisplaced intercondylar
fractures.
Interlocking
nails have been used successfully to treat high supracondylar fractures of the
femur and segmental fractures of the femur with supracondylar
components.85,190,350,379 The applicability of this technique to ipsilateral
fractures of the shaft and distal femur depends on whether the distal screws of
interlocking nails can provide fixation of both the femoral shaft fracture and
the supracondylar and intercondylar fractures. Therefore, this technique is
dependent on the fracture pattern. Lateral and oblique radiographs of the
distal femur are recommended to rule out fractures of the femoral condyles in
the coronal plane (the so-called Hoffa fracture). Because the plane of these
fractures parallels the interlocking screws, reduction and stabilization of
this fracture variant by interlocking nailing is tenuous, and other methods
should be selected.
The
intercondylar fracture must be stabilized initially with cancellous lag screws
placed anteriorly or posteriorly in the femoral condyles. Anatomical reduction
of the articular fracture is imperative and may necessitate open reduction.
Open reduction through a parapatellar arthrotomy provides the best visualization
of the fracture site. Nondisplaced fractures can be treated with percutaneous
cancellous screw fixation under image intensifier control (Fig. 27-40 and Fig.
27-41). Our experience with a limited number of these fractures indicates that
rotational malalignment of the femoral condyles is common, and an arthrotomy
should be performed to check visually the reduction of the articular surfaces.
Central placement of the screw in the condyles will obstruct the passage of the
interlocking nail, leaving the distal interlocking screws too proximal for
adequate condylar fixation. The preferred number of lag screws depends on the
fracture pattern. The nailing should be performed after fixation of the
intercondylar fracture with two screws to prevent possible displacement of the
intercondylar fracture. If further lag screw placement is needed, it should be
performed after nail insertion. Standard interlocking nailing then is performed
carefully, with attention paid to reaming into the intercondylar portion of the
femur. This reaming is necessary to prevent spreading of the intercondylar
fracture on insertion of the nail. An intramedullary nail of sufficient length
to extend down to the subchondral bone of the intercondylar notch is inserted
so that the distal interlocking screws act to stabilize both the intercondylar
fracture and the interlocking nail to the distal femur. Because the stability
obtained with this method depends on the fracture geometry and the purchase of
the lag and locking screws, the postoperative rehabilitation must be
individualized to each injury. Weight bearing on intercondylar fractures should
be postponed for at least 6 weeks after fixation.
If
the distal fracture is too comminuted or too low, or if it has fracture lines
in the coronal plane, then fixation with this method is contraindicated. Open
reduction and plate fixation are used in such cases. Acceptable results have
been reported with both the open plating and interlocking nailing with adjuvant
screw fixation techniques in these rare injuries.66,374
Pathologic Fractures
Pathologic
fractures involve the femoral shaft much less frequently than they do the
proximal femur. Most are transverse or short oblique fractures sustained with
minor violence. Pathologic fractures should be suspected if there is any
scalloping or erosion of the cortex at the fracture site. The history of minor
trauma along with the radiographic evidence of pathologic bone usually leads to
a presumptive diagnosis of pathologic fracture. Excluding osteoporosis, most
pathologic fractures are secondary to metastatic disease. Primary benign and
malignant tumors of the femoral shaft are rare.
Pathologic
fractures entail both diagnostic and therapeutic challenges. If the primary
diagnosis is unknown, biopsy is mandatory. A biopsy technique should be
selected that minimizes any seeding of the adjacent tissues with tumor.
Biopsies of most metastatic tumors are taken at the time of skeletal fixation.
As with all bone tumors, careful histologic and radiographic correlation is
needed for a correct diagnosis.
The
goal of treatment, especially for fractures through metastases, is rigid
stabilization of the femur, affording immediate pain relief and early weight
bearing. Prompt surgical stabilization of pathologic fractures facilitates
nursing care, reduces hospital costs, and provides a beneficial psychological
effect on the patient. If no preexisting oncology-related problems, such as
hypercalcemia, dehydration, or pulmonary insufficiency, are present, surgery
should be performed as expeditiously as possible. Traction and cast bracing
necessitate prolonged bed rest without predictable pain relief or healing of
the pathologic fracture. Plating is associated with slow healing and requires
prolonged protection from weight bearing (Fig. 27-42). The open exposure of
plating risks major hemorrhage in certain highly vascular tumors. Further
growth of the tumor also can compromise plate fixation.
Despite
these limitations of plating, satisfactory functional results have been
reported. Broos and associates49 used anterior and lateral plates supplemented
with polymethylmethacrylate to stabilize ten pathologic fractures of the
femoral shaft. In their combined series of 48 pathologic femoral fractures, 75%
of patients recovered the ability to walk. These investigators considered
contraindications to surgical stabilization to include a survival expectancy of
less than 4 weeks, a premorbid general condition that precluded a safe general
anesthesia and surgery, and complete mental deterioration of the patient to the
point at which pain relief was not an issue.
Intramedullary
nails achieve most of the therapeutic goals for pathologic fractures. Small,
well-localized lesions near the isthmus are manageable with conventional nails.
Large lesions with extensive bone loss, lesions proximal or distal to the
isthmus, and multiple lesions in the shaft require adjunctive fixation with
locking screws or polymethylmethacrylate. A variety of techniques have been
described for the use of bone cement.181 Whatever construct or technique is
used, rigid fixation must be the goal. Intramedullary nails do not preclude the
early use of radiation therapy for shrinkage of the tumor. The Zickel nail is
especially well designed for pathologic fractures in the subtrochanteric
region.
In a
series of 43 femora with metastatic lesions, Sangeorzan and colleagues305
reported good results with prophylactic Zickel nailing of impending
subtrochanteric and proximal shaft fractures. A modified closed nailing
technique was used to minimize blood loss and operative time. Eighty percent of
the patients walked on the leg within 4 days after the nailing. The average
length of survival after surgical stabilization is 9 to 12 months in most
published series.49,305
Controversy
still surrounds the issue of the need and timing for prophylactic nailing of
metastatic lesions without fracture of the shaft (Fig. 27-43). Radiographic
guidelines have been developed based on retrospective clinical studies.221
Prophylactic nailing is recommended if (1) the ratio between the width of the
metastasis and the bone is greater than 0.6, (2) the axial cortical destruction
is greater than 30 mm in length, or (3) the cortical destruction is greater
than 50% of the circumference of the shaft. Smaller lesions in the
subtrochanteric region are especially likely to act as stress risers for
pathologic fractures (Fig. 27-44).
Pathologic
fractures also can be due to Paget disease.129 The femur is the most common
bone fractured in Paget disease. The usual transverse fracture located in the
subtrochanteric or proximal third level of the bone occurs most frequently in
the late stages of the disease. Fractures in the early stages of Paget disease
may hemorrhage excessively. The treatment of pagetoid fractures can be difficult.
Traction treatment is associated with varus malunion and refracture.129
Intramedullary nailing is preferred in most cases but can be technically
demanding. A short nail may be required to prevent penetration of a deformed
shaft. Fracture healing, however, proceeds rapidly. In the presence of severe
deformity of the shaft, other treatment options, including corrective
osteotomies, plates, or traction, can be chosen.
Fractures in
Elderly Patients
Although
proximal femoral and distal femoral fractures far outnumber femoral shaft
fractures in elderly patients, the incidence of shaft fractures in this group
is increasing with the aging of the American population. Most shaft fractures
in the elderly are caused by low-velocity injuries from falls at home.
Associated injuries are few. The osteopenic cortical bone often is comminuted
despite the low-velocity mechanism of injury.235 The goal of treatment is
similar to that of hip fractures in the elderly and should include sufficiently
rigid fixation of the fracture to allow full weight bearing on the leg. The
osteopenic diaphysis with a large medullary canal is not amenable to
stabilization with either plating or external fixation, and intramedullary
nailing appears to offer superior functional results over other forms of
fixation.6,151,235
Moran
and coworkers,235 in a series of 24 patients with a mean age of 77 years, noted
rapid healing of femoral shaft fractures treated with statically locked nails.
They used large-diameter nails in their patients, nearly all of whom were
women. As would be expected in such an elderly population, perioperative
complications, including decubitus ulcers, urinary tract infections, and
congestive heart failure, were common, and 4 of the 24 patients died after
surgery. Alho and associates6 reported similar results, with an additional
complication of postoperative shortening of the femur by more than 2 cm in more
than half their 15 patients treated by dynamically locked nails.
Perioperative
complications from intramedullary nailing of shaft fractures in elderly
patients can be minimized by careful adherence to several technical principles.
The status of the ipsilateral hip joint must be assessed by perioperative
radiographs because many elderly patients have preexisting hip pathology. Moran
and coworkers identified 5 of their 24 patients as having either osteoarthritis
or previous hip fracture that limited hip adduction and required modification
of patient positioning during nailing of the shaft fracture. One of the
patients had marked bowing of the shaft, which also necessitated a change in
the nailing technique. The capacious canal is filled best with a large-diameter
nail, and static locking is imperative to prevent shortening around the nail.
Distal locking screw purchase can be compromised by the osteopenic bone in the
distal femoral metaphysis. Fully threaded locking screws are preferred, and a
locking bolt on the medial end of the screw can prevent postoperative loosening
and backout of the screw. Moran and coworkers235 supplemented their distal
locking screws with intramedullary polymethylmethacrylate in several cases.
Late
complications after nailing also are more common in elderly patients. The
large, stiff nail can create a stress riser effect in the proximal femur and predispose
to subsequent femoral neck or peritrochanteric fracture.235 Careful placement
of the entrance portal and precise reaming of the canal lessen the likelihood
of such proximal femoral fractures.
Gunshot
Fractures
Gunshots are a
common mechanism of injury for femoral shaft fractures in most large urban
communities. Most are small-caliber, low-velocity injuries. The effect of a
small-caliber missile on the tubular bone of the diaphysis is different from
that on metaphyseal bone.
Four
fracture patterns have been identified after gunshot wounds to the femur.325
The 'drill hole' fracture characteristically occurs in the distal
femoral metaphysis secondary to a direct impact of the missile on the
cancellous bone. The butterfly fracture results from a direct hit of the bullet
on the diaphysis with variable degrees of cortical comminution. An incomplete
fracture is caused by nicking or incomplete bone penetration of the missile. In
this last fracture, the impaction of a small cortical fragment can weaken the
bone even though the femoral diaphysis is sufficiently intact to allow for full
weight bearing. The fourth pattern is a spiral fracture, which can occur
proximal or distal to one of the three other patterns. Although this fracture
traditionally has been attributed to the fall that some patients report after
being shot, it probably is due to a stress riser operating on the loaded femur
at remote distances from the site of missile impact.325
For
most gunshot fractures of the femoral shaft, the preferred treatment is the
same as if the fracture were closed.43 No formal debridement of the fracture
site or coring of the entrance hole is necessary.149 Closed interlocking
nailing is performed in a standard fashion. The preferred timing for nailing is
unaffected by the presence of the bullet tract, although other gunshot injuries
to the thorax, abdomen, or head may alter the timing of nailing. The results
are comparable to those obtained with closed fractures28,192,375 (Fig. 27-45).
Infection rates are similar to those seen after nailing of closed fractures.
Immediate nailing of these fractures decreases the cost of hospitalization and
subsequent care in this often unreliable patient population.28,192 The
principles of management of high-energy gunshot injuries differ significantly.
High-velocity rifle injuries and close-range shotgun blasts are associated with
extensive soft-tissue cavitation and necrosis, and, therefore, should be
considered grade III open fractures. Thorough debridement of the fracture with
removal of all foreign material and open wound care are imperative. External
fixation or traction is indicated if the soft-tissue wound is extensive and
bone is exposed in the open wound. Delayed internal fixation after soft-tissue
coverage facilitates fracture management in selected cases.43
INTRAMEDULLARY NAILING: TECHNIQUES AND PITFALLS
Timing of Surgery
The relative
merits of early versus delayed nailing for femoral fractures have been studied
extensively over the last 40 years. Early work suggested more rapid fracture
healing with delayed fixation.80,185,326 Other studies refuted these
claims,107,256 and most recent clinical and laboratory investigations support
the concept that delaying the timing of intramedullary nailing has no
beneficial effect on fracture healing.
A
more salient argument for early nailing is its advantageous effect on prompt
patient mobilization and pulmonary function, especially in the multiply injured
patient.
Retrospective
investigations by Goris,122 Meek,218 Johnson,161 Riska,288,289 and Seibel314
and their colleagues demonstrated improved survival for the multiply injured
patient who received fracture fixation within 24 hours of injury. The
improvement resulted from a lower prevalence of sepsis due to a decrease in the
rate of pulmonary insufficiency. Lozman and associates199 reported a randomized
prospective investigation that verified the beneficial effects of early
fracture fixation with respect to the pulmonary and cardiovascular systems. Poole and coworkers272 found no increased risk of pulmonary or cerebral complications from
early femoral fixation in a series of patients with head trauma and long-bone
fractures.
Bone
and colleagues34 published the results of a randomized prospective study at Parkland Memorial Hospital on both isolated femoral fractures and femoral fractures in
patients with multiple organ system injury. All patients had femoral shaft
fractures and received either early or delayed fixation. No patient with an
isolated femoral fracture (ISS á 18) had pulmonary insufficiency, but 23% of
those with isolated injuries treated by delayed fixation (more than 72 hours
after injury) had abnormal arterial blood gases as compared with 10% of those
whose fractures were stabilized within 24 hours. The length of hospital stay
and hospital costs were decreased in the immediate fixation group. In the
multiply injured population, the differences between the immediate and delayed
stabilization groups were even more pronounced. Compared with those treated
with delayed fixation, multiply injured patients undergoing immediate femoral
stabilization had lower prevalences of pulmonary insufficiency and adult
respiratory distress syndrome, fewer days in the intensive care unit, fewer
days on ventilatory support, shorter hospital stays, and lower total costs for
inpatient care.
Reaming
of the femoral nail results in increased intramedullary pressure and variable
amounts of embolization of bone marrow contents to the lungs. Wenda and
colleagues360 measured increases in intramedullary pressure up to 200 to 600 mm
Hg during reamed nailing compared with only 70 mm Hg during nonreamed nailing.
The triglycerides and other marrow elements cause the release of various
mediators in the lungs that increase pulmonary capillary permeability.260,261,360
The magnitude of the embolization as measured by echocardiography appears to be
much greater when reamed nailing is performed compared with nonreamed
nailing.253,360 No clinical studies have documented the importance of these
observations on the pulmonary function of patients, but they have led some
investigators to recommend the routine use of nonreamed nails, especially in
multiply injured patients.12,261 Until further studies clearly demonstrate a
better risk-benefit profile for nonreamed nails, reamed nailing remains our
preferred technique. The results of all these studies over the last 25 years
make it apparent that immediate fixation of femoral shaft fractures provides
the optimal environment for patient recovery.97,122,199 Immediate fixation of
femoral shaft fractures at our institutions is preferred for isolated shaft
fractures and is mandatory, except in the most extenuating of circumstances,
for femoral fractures in the multiply injured patient.
Preoperative Planning
The clinical
results of closed interlocking nailing are largely a function of meticulous
preoperative and intraoperative planning. As with any complex surgical
procedure, close attention to details is imperative for a successful result.136
Weller and coworkers359 poetically noted that 'most complications happen,
when the surgeon-either pressed by time or out of an unjustifiable artistic
liberality-deviates from the regular technique.' Preoperative anticipation
of technical problems can save the surgeon considerable time in the operating
room.
Diagnostic
radiographs must be of sufficient quality to assess the extent of fracture
comminution. Longitudinal fissures in the proximal or distal fracture fragments
can be missed with suboptimal radiographs (see Fig. 27-21). Such nondisplaced
comminution can influence the choice of locking screws or, in cases of
fractures extending into the hip or knee joints, the preferred fixation
implant. Biplanar radiographs of the knee and an anteroposterior radiograph of
the pelvis are part of the standard evaluation of a femoral shaft fracture and
assist in ruling out associated hip injuries and ligamentous injuries around
the knee.
The
geometry and dimensions of the femur can be assessed on the plain radiographs.
The medullary width of the isthmus on the anteroposterior radiograph is a good
measure of the probable width of the nail to be used. For simple Küntscher
nailing, a nail with a diameter 2 mm greater than the radiographic medullary
diameter is optimal. Filling of the medullary canal is less critical in cases
in which static interlocking nailing is required.
Preoperative
measurements of femoral length and the ideal length of the anticipated nail are
necessary. Inadvertent lengthening or shortening of the femur during nailing
can occur easily, especially in Winquist type IV comminuted fractures. Clinical
measurement of the contralateral uninjured femur from the tip of the greater
trochanter to the lateral aspect of the knee joint provides useful surface
landmarks for correct length. Radiographic measurement of the contralateral
femur with a nail of known length taped to the lateral surface of the thigh
yields a more precise determination of normal femoral length. With this
technique, problems with radiographic magnification are obviated, and both the
preferred length of the nail and its precise depth of insertion into the distal
fragment are easily calculated. Alternatively, the Küntscher ossimeter, which
corrects for radiographic magnification, can be used. Some interlocking nailing
systems offer radiographic templates that can be used for measuring nail size
and position for complex fracture patterns. A stock of standard cloverleaf
nails and interlocking nails of at least 4 cm greater and lesser length and of
at least 2 mm greater and lesser width than the preoperative measurements
should be available in the operating room (Fig. 27-46).
If
closed nailing is not to be performed on an emergent basis, the patient's leg
is placed in balanced suspension traction using a proximal tibial pin. Preoperative
distraction of the major fracture fragments should be ensured by the
application of 25 to 40 lb of traction weight. If surgery is postponed for more
than 3 to 5 days, radiographic documentation of fracture distraction using a
lateral radiograph of the femur is advisable. Simple transverse fractures with
spiked bone ends are especially difficult to reduce if surgery is delayed, and
overdistraction of the fracture fragments of at least 5 to 10 mm should be
sought.
A
systemic antibiotic, usually a first- or second-generation cephalosporin, is
administered 30 minutes before skin incision and is continued for 24 hours
after the surgery.
Patient Positioning
After the
induction of general anesthesia, careful attention must be focused on patient
positioning on the fracture table. Correct patient positioning often makes the
difference between a successful and an unsuccessful nailing. If difficulty in
achieving a closed reduction using a tibial pin is anticipated, a distal
femoral pin should be inserted before positioning of the patient. Distal
femoral shaft fractures are especially troublesome to reduce with tibial
traction because of the deforming effects of the gastrocnemius muscle and the
posterior knee capsule. A distal femoral Steinmann pin is inserted as far
distal and anterior in the femoral condyles as feasible, thereby permitting
direct longitudinal traction on the distal fragment without interfering with
placement of the distal locking screws. Fluoroscopic guidance of this distal
femoral pin is advisable to prevent penetration into the knee joint. If this
pin blocks full insertion of the nail into the distal fragment, or placement of
the distal screws, it can be extracted safely after partial insertion of the
nail into the canal of the distal fragment. A traction bow similar to that used
for skull traction and a modified technique using half-pins as joysticks also
have been recommended for very distal fractures.350
Femoral
nailing can be performed with the patient in either the supine or lateral position
on the fracture table.1 The supine position is preferable in patients with
multiple injuries, especially associated pulmonary injury, unstable spine or
pelvic fractures, or contralateral femoral fracture (Fig. 27-47). The supine
position also is preferred for the insertion of second-generation nails when
unobstructed visualization of the femoral head and neck on anteroposterior and
lateral fluoroscopy is needed. Ventilatory assistance of patients with
compromised pulmonary function can be impaired if a lateral position is used. A
lateral position also can increase the risk of fracture displacement and
further soft-tissue damage in patients with unstable pelvic and spinal
injuries. However, access to the entrance portal of the nail in the
trochanteric fossa often is limited using the supine position. The lateral
position permits easy exposure of the entrance portal but does require slightly
more time for patient positioning. Obese patients are ideal candidates for the
lateral position.
Closed
reduction is achieved easily with the supine position, and problems of rotatory
malalignment are encountered less frequently than with the lateral position.
The trunk and pelvis of the patient are tilted away from the injured leg,
providing a degree of adduction of the hip. The affected hip is flexed about
15° and the opposite leg is extended. The vertical post stabilizes the pelvis
and the proximal femur. Satisfactory rotatory alignment is achieved in most
cases by allowing the suspended leg to hang perpendicular to the floor.
Attempts to judge the correct rotation based on the radiographic appearance of
the fracture fragments usually are inaccurate. If necessary, the anteversion
can be assessed on the fracture table, and the distal fragment can be rotated
to restore the normal torsion of the femur. Proximal-third fractures tend to
angle in varus orientation with the patient supine on the table, and
adjustments in patient positioning, including switching to the lateral
decubitus position, may be necessary in such cases. A long incision often is
required for adequate exposure, especially in obese patients.
When
the lateral position is chosen, both vertical and longitudinal posts on the
Maquet table are used to hold the pelvis during the reduction and nailing of
the femur. The hip is slightly adducted and moderately flexed to improve the
reduction of the fracture and enhance access to the trochanter. Traction is
applied through the proximal tibial or distal femoral pin with the knee flexed
a minimum of 60°. Traction through a foot plate with the knee extended can
stretch the sciatic nerve and should be avoided. Internal rotation of 10° to
15° in relation to the floor usually guarantees correct rotatory alignment of
the fracture fragments. A common error is to allow the leg to rotate externally
on the fracture table, resulting in a 20° to 30° external rotational
malalignment. Although most patients will accept this degree of malrotation,
every effort should be made to prevent it. Extension of the contralateral leg
allows for unimpeded free movement of the C-arm of the image intensifier (Fig.
27-48).
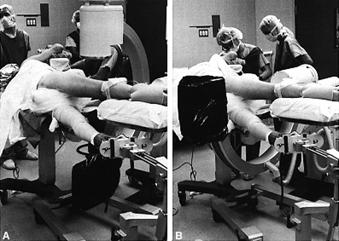
Fig.
27-48
Satisfactory
reduction of the fracture must be obtained in both the anteroposterior and
lateral planes before preparation and draping of the leg. In the lateral
position on the table, the proximal fragment tends to flex and adduct in
relation to the distal fragment. A crutch can be used to support the proximal
fragment and correct any residual mediolateral angulation or displacement.
Gentle pressure with a crutch or lead-gloved hand is applied on the anterior
thigh to confirm that any anteroposterior translation at the fracture can be
corrected. Any residual minor displacement of the fracture fragments can be
reduced during surgery. If near-anatomical reduction is not radiographically
evident, however, adjustments in the position of the patient and the extremity
must be made before draping. It may be necessary to release the traction and
perform a formal manipulation of the extremity. Sufficient traction for slight
distraction of the fracture aids in achieving reduction and passage of the
guide pins. If cyanosis or mottling occurs in the leg, pressure on the anterior
aspect of the hip by the vertical post should be relieved.
An
alternative nailing technique without the use of a fracture table has been
recommended for selected fractures.24,214 Distraction of the acute fracture is
accomplished through half-pins inserted into the proximal femur and the femoral
condyles using an AO femoral distractor. Anatomical studies demonstrate that
the proximal pin can be placed safely distant from the femoral artery and nerve
and still not block the insertion of the nail. Although reduction must be
achieved by manipulation during the procedure, satisfactory alignment can be
obtained in most cases. This technique can be useful for multiply injured
patients in whom the manipulation of positioning on the fracture table involves
major risk. It is uncommon, however, for concomitant injuries to be of such
severity as to preclude the safe use of a fracture table.
Poor
patient positioning before preparation and draping of the limb can create
numerous intraoperative problems. It is advisable to spend whatever additional
time is required to ensure that a reduction and distal targeting are
achievable.
Reaming and Nailing Maneuvers
Excessive
radiation exposure to the surgeon's hands and body are a major concern with
closed intramedullary nailing. Studies have shown that the greatest dose of
radiation to the dominant hand occurs during nail insertion and distal
targeting.91,191 Although the total accumulated dose is low, every effort
should be made to minimize the use of fluoroscopy during reduction, reaming,
nailing, and locking of the fracture. Lead aprons and thyroid shields, along
with lead-impregnated glasses, are always advisable. Continuous imaging during
nailing and locking is unnecessary, and split-second spot images suffice. The
x-ray tube should not be in proximity to the patient because this enhances the
scatter radiation to the surgeon. The surgeon and assistants should stand back
away from the image intensifier whenever live imaging is being performed.
The
lateral incision extends from 1 cm distal to the tip of the greater trochanter
superiorly for 8 to 10 cm. If proximal locking is anticipated, the incision is
carried distally an additional 3 to 4 cm. Longer incisions are required in
patients with bulky soft tissues. The fascia lata and the fibers of the gluteus
maximus are divided in line with the skin incision. The interval between the
abductor tendon insertion on the greater trochanter and the pyriformis tendon
is identified, and the gluteus medius and minimus are freed from the underlying
hip capsule. The trochanteric or piriformis fossa is visualized by retraction of
the abductor muscles anteriorly.
Accurate
positioning of the entrance hole is critical.165 The anterior bow of the shaft
curves up to the posterior tip of the greater trochanter. Therefore, the
beginning awl should be inserted just posterior to the midline of the
trochanter and just medial to the prominence of the trochanter in the
trochanteric fossa (Fig. 27-49). Such placement ensures that the hole will be
aligned with the longitudinal axis of the medullary canal in both the sagittal
and coronal planes. An entrance portal anterior to the midpoint of the
trochanter can result in perforation of the anterior cortex of the proximal
femur. A laterally placed portal at the tip of the trochanter frequently leads
to eccentric reaming and medial comminution of the proximal fragment. Varus
malalignment of the fracture, especially in proximal shaft fractures nailed
with the patient in a supine position, also can be a complication of an
entrance hole in the trochanteric tip. Varus reduction is observed commonly in
second-generation reconstruction nailing of proximal femoral fractures and can
result in errant placement of the locking screws high in the femoral head.
Medial placement of the entrance portal must be prevented in adolescent
patients, who may be prone to osteonecrosis of the femoral head secondary to
iatrogenic damage to the vascular arcade at the base of the femoral neck.
Excessive medial placement of the awl can create a stress riser in the femoral
neck. After full insertion of the diamond-tipped awl, its position should be
visualized in both planes with the fluoroscope. Any deviation from the
trochanteric fossa must be corrected before reaming of the canal. When the
supine patient position is used, the entrance hole can be difficult to make
with a sharp-tipped awl. A Steinmann pin can be drilled into the proximal femur
under image intensifier control in such cases and the hole made over the pin
with a cannulated reamer.105

Fig.
27-49
Initial
reaming of the proximal fragment is performed with the 6-to 9-mm hand reamers.
This preliminary reaming improves the freedom of movement of the bulb-tipped
guide pin as it is being passed into the medullary canal of the distal
fragment. The guide pin is controlled with a T-handle chuck. Passage of the guide
pin across the fracture site into the distal fragment can be facilitated by a
small curve at the tip of the guide pin (Fig. 27-50). If residual translation
of the fracture fragments is present, direct external pressure on the thigh
with a crutch or lead-gloved hand may be needed. Alternatively, a
small-diameter (8- to 10-mm) Küntscher nail inserted into a previously reamed
proximal fragment can be manipulated as a lever to improve alignment with the
guide pin inserted through the nail. Commercially available cannulated guides
also are available to control the proximal fragment during guide pin insertion.
Passage of the guide pin into the distal fragment by one or more of these
reduction maneuvers is almost always possible. Open reduction for guide pin passage
should be reserved for the rare case of an irreducible fracture or
incarceration of bone fragments in the medullary canal.

Fig.
27-50
Fractures
of the distal third of the shaft pose a special reduction problem. In the
supine position, the distal fragment angles posteriorly and must be supported
with a crutch or by an unscrubbed assistant. In the lateral position, the
distal fragment sags into valgus angulation. If full correction of this
angulation is not achieved before guide pin insertion, the nail may be driven
into the medial femoral condyle, resulting in an unsatisfactory valgus
malalignment, or into the lateral femoral condyle, resulting in a varus
malalignment. The guide pin should be aimed directly at the intercondylar notch
on the anteroposterior view of the femur before reaming and nailing of the
distal fragment. Radiographic verification of proper pin position in both
planes is imperative at this stage of the operation.
After
full insertion of the guide pin, the length of the remaining pin is measured
from its tip to the trochanter and subtracted from the total length of the
guide pin. Using the preoperative measurement of ideal nail length along with
this measurement, the preferred-length nail is chosen. For Winquist type IV comminuted
fractures, adjustments in the longitudinal traction may be needed to restore
the femur to its normal length.
Flexible
reamers, starting with a 9-mm end-cutting reamer, are used to enlarge the
medullary canal (Fig. 27-51). The reamers are passed across the isthmus until
no further resistance is encountered. Reaming of the distal fragment down to
the anticipated distal tip of the nail is unnecessary and can compromise the
purchase of the nail on the cancellous bone of the distal third of the shaft. If
there is a segmental bone loss or comminution in the shaft, the reamers should
be pushed, not powered, across the defect to prevent any damage to the soft
tissues of the thigh. Reaming proceeds at 0.5-mm increments until endosteal
cortical contact of the reaming heads over a segment of 2 to 3 cm of both the
proximal and distal fragments is achieved. Such cortical contact is not
feasible or necessary for proximal and distal shaft fractures, which are
stabilized with interlocking nails. The canal is overreamed at least 0.5 mm for
simple cloverleaf nails and 1 mm for interlocking nails. Failure to ream the
canal to a diameter slightly greater than that of the nail can result in nail
incarceration or iatrogenic comminution of the fracture. Distal-third fractures
especially require a minimal 1- to 1.5-mm overreaming of the proximal fragment
to accommodate the variable degree of anterior femoral bow that might be
present. If the reaming head jams in a tight canal, it can be extracted by
driving it out with the bulb-tipped guide pin. External pressure on the thigh
for fracture alignment is helpful to prevent eccentric cortical reaming during
passage of the reamer into the distal fragment. At the completion of reaming,
the 3-mm bulb-tipped guide pin is exchanged for the 4-mm straight guide pin
through a plastic medullary tube.
The
design of the medullary reamer can be important in influencing the amount of
marrow embolization to the lung during the reaming maneuver. In an intact femur
model in sheep, Pape and colleagues261 showed that the AO reamer design
resulted in a significant increase in pulmonary artery pressure and pulmonary
capillary permeability damage compared with other reamers. These transient
changes in the lungs were attributed to the cylindrical design of the AO
reamer, which tends to occlude the canal (Fig. 27-52). Improvements in reamer
design should be forthcoming soon.
In
the presence of segmental bone loss after an open fracture, transmedullary bone
grafting during delayed nailing occasionally is indicated. Bone particles
removed during the reaming maneuver are mixed with autogenous cancellous bone
graft from the iliac crest. This morselized graft can be inserted through a
chest tube and deposited throughout the area of bone loss before nail insertion.
The
preselected interlocking nail then is driven over the 4-mm nail guide pin into
the proximal fragment. Perfect correction of fracture alignment is necessary as
the nail is passed across the fracture into the distal fragment. The handle on
the driver is held firmly to ensure that the prebent curve of the nail is
aligned properly with the anterior bow of the femur. Once the nail has entered
the canal of the distal fragment for a distance of 3 to 4 cm, the rotatory
alignment of the limb is checked and the traction is adjusted to restore normal
femoral length. The nail then is driven fully into the distal fragment until
the lateral flange of the driver or the proximal targeting jig impacts on the
tip of the greater trochanter. The diagonal hole of the interlocking nail
should be centered on the intertrochanteric region, and the distal holes should
be aligned in the coronal plane. Incomplete insertion of the nail results in
errant placement of the proximal locking screw into the femoral neck. If the
distal holes of the nail are aligned more in the sagittal plane, elastic or
plastic deformation of the nail in torsion may have occurred during its
insertion into a tight canal. Such torsional deformity of the nail occurs more
frequently with thin-walled, slotted nails. More overreaming of the canal or
exchange to a smaller-diameter nail is indicated in such cases.
Proximal Locking
The decision to
lock the proximal fragment, the distal fragment, or both to the nail is based
on the preoperative and intraoperative assessment of the fracture. If the
fracture is too far proximal, too far distal, too oblique in its anatomy, or
too comminuted to be afforded stability by an unlocked cloverleaf nail, then
locking screws are indicated. The broad guidelines recommended by Winquist and
coworkers370 are used at our centers (Fig. 27-53). Studies at the Shock Trauma
Center have demonstrated that it is wise to err on the side of locking whenever
there is any doubt about the stability provided by an intramedullary nail.59,60
It is apparent that fixation with static interlocking reduces the prevalence of
postoperative fracture complications without increasing the low risk of femoral
nonunion. At our centers, only the simplest, transverse midshaft fractures are
considered appropriate for nailing without static locking of the major fracture
fragments.
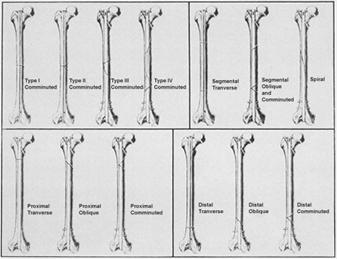
Fig. 27-53 Terapia preferata in
fracturi de diferite tipuri functie de anatomie, localizare si
cominutie.
Proximal
locking is performed easily using a proximal targeting device that attaches
firmly to the proximal tip of the nail. This targeting jig must be screwed
tightly into the internal thread at the proximal tip of the interlocking nail.
Most interlocking nails are designed for a 6-mm fully threaded screw that
passes diagonally from the greater trochanter to the lesser trochanter at a 45°
angle to the nail. The near cortex is overdrilled to 6 mm, whereas the far
cortex at the level of the lesser trochanter is drilled to 5 mm. A fully
threaded, fluted screw of appropriate length then is inserted. If the nail is
manufactured with an internal thread for this screw, then resistance is
encountered as the screw is passed through the nail. The screw must be
sufficiently long to gain a firm purchase of the far cortex. Insertion of this
diagonal screw is predictable as long as the targeting device is attached
snugly to the proximal end of the nail.
Distal Locking
Distal locking
for control of length, rotation, or both of the distal fracture fragment is
performed in nearly all cases. It is the major technique, over and above
standard closed nailing, that must be mastered for a successful interlocking
nailing. Over the last decade, several distal targeting techniques have been
introduced, tested, and often discarded.31,135,217 Nail-mounted targeting jigs
are available with most interlocking systems. Both the Grosse-Kempf and the
Russell-Taylor nails possess internal threads in the proximal tip of the nail
to which the jig is attached. Theoretically, the device can be preassembled
before nail insertion so that, when it is reattached after nail insertion,
perfect alignment of the jig with the holes is achieved. However, deformation
of the nail during insertion invariably makes adjustment of the holes of the
jig under fluoroscopic guidance necessary. The time needed for such adjustment
can be lengthy, and even with precise alignment of the holes of the jig and the
nail, slight movements of the jig during drilling of the holes often cause
errant placement of the holes. Most nail-mounted targeting devices have been
replaced by alternative techniques for distal targeting.50,51,202
Various
hand-held targeting devices also are available (Fig. 27-54). Most involve a
drill sleeve attached to a long handle that often is radiolucent. The drill
sleeve is introduced down to the lateral cortex through a small percutaneous
wound over the lateral thigh. Fluoroscopic alignment of the nail hole with the
drill sleeve permits accurate targeting. Because of the sloping surface of the
distal femur and the long handle of the targeting device, a delicate touch is
required to prevent loss of precise positioning.
We
perform most of our distal targeting using a free-hand technique. A 3- to 4-cm
incision is made in the lateral thigh directly over the two distal holes of the
nail. The iliotibial band is split in line with the skin incision, and the
vastus lateralis muscle is retracted anteriorly off the intermuscular septum.
Sufficient periosteum is elevated off the cortex to permit unimpeded use of the
awl and drill. The radiology technician adjusts the position of the C-arm to
align the radiation beam perfectly with one of the distal holes. A perfect
circle should be visualized through the hole. The tip of a straight,
long-handled awl is rested on the lateral cortex so that its point lies in the
center of the hole (Fig. 27-55). The fluoroscope is turned off, and the shank
of the awl is brought up directly in line with the C-arm.191 Constant pressure
is maintained on the awl handle to prevent skidding of the awl tip on the bone.
With the use of a mallet, the tip of the 6-mm-diameter awl is driven through
the lateral cortex into the hole of the nail. Repeated fluoroscopic imaging
confirms accurate placement of the awl (Fig. 27-56). The awl is removed, and a 4.5-
or 5-mm drill bit is used to drill the far cortex (Fig. 27-57). Alternatively,
the drill bit can be used primarily to center the hole without using the awl.
Most interlocking systems provide either partially or fully threaded,
self-tapping, 5- to 6.25-mm screws for distal locking (Fig. 27-58).
Two
distal screws are inserted routinely to prevent toggling of distal fractures in
the sagittal plane. Biomechanical studies have demonstrated, however, that
there is no significant difference in the torsional rigidity or axial load to
failure when one as opposed to two distal 6-mm screws are used with slotted
nails for midshaft or proximal fractures.133 Limited clinical studies confirm
the adequacy of a single locking screw for most proximal and midshaft injuries,
although migration of the simple distal locking screw can occur.133 If any
doubt concerning the stability of fixation exists, two locking screws are
preferred.
Surgical Technique for Reconstruction Interlocking Nailing
The
second-generation, or reconstruction, nails were developed to address the
unique anatomical and biomechanical demands of complex femoral fractures,
including subtrochanteric fractures, impending pathologic fractures of the
proximal femur, and ipsilateral femoral shaft and neck fractures. All such
nails are designed to permit the placement of one or more screws into the
femoral head and neck. The Russell-Taylor reconstruction nail is typical of
these second-generation nails. Its proximal sliding screws neutralize
rotational and shear forces and provide excellent purchase of the femoral head
and neck. The closed-section design of this nail decreases torsional shear at
the fracture site and reduces torsional rotation of the nail during insertion.
Small-diameter (delta) reconstruction nails have an increased wall thickness
that enhances their bending strength. The proximal 8 cm of all reconstruction
nails have an expanded diameter to provide the additional strength needed for
the proximal lag screws. The two self-tapping, partially threaded proximal
screws are 8 and 6.4 mm in diameter, respectively. Sliding of these screws
within the holes in the nail is possible to accommodate any postoperative
settling of a peritrochanteric or neck fracture.
The
surgical technique for standard interlocking nailing must be modified in
several important ways for successful insertion of the reconstruction nail. The
patient positioning must be supine to allow for unobstructed fluoroscopic
visualization of the anteroposterior and lateral projections of the femoral
head and neck (Fig. 27-59). The involved leg is adducted and slightly flexed on
the fracture table, whereas the contralateral leg is positioned either in
extension and abduction or in flexion and external rotation to permit unimpeded
movement of the image intensifier. With a distal femoral traction pin,
rotational alignment of the femur usually is restored by allowing the knee to
flex with the foot pointing to the floor.
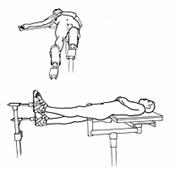
Fig.
27-59
Through
the standard incision and approach, the curved awl or cannulated reamer is
introduced into the trochanteric fossa. High subtrochanteric fractures are
subjected to deforming muscle forces that often abduct the proximal fragment. A
bone hook on the tip of the greater trochanter or a commercially available
cannulated alignment device can be used to adduct the trochanteric fragment,
thereby avoiding varus nailing of the fracture. If the reconstruction nail is
being used for an ipsilateral femoral neck and shaft fracture, preliminary
reduction and provisional screw or pin stabilization of the neck fracture
should be performed before the reaming and nailing maneuvers.
After
insertion of the bulb-tipped guide rod, precise determination of the preferred
nail length must be calculated. The depth of the chosen nail may have to be
adjusted to ensure accurate placement of both proximal screws, so careful
selection of a proper-length nail is imperative. The medullary canal then is
overreamed a minimum of 1 mm greater than the selected nail diameter. The
proximal 8 cm of the proximal femur is reamed to 15 mm for the expanded portion
of the reconstruction nail.
The
nail then is inserted to the proper depth to allow for placement of both
proximal screws in the femoral head and neck. This depth can be determined by
placement of the drill sleeves into the proximal drill guide and extrapolation
of the eventual location of the screws by fluoroscopic inspection of the
position of the sleeves (Fig. 27-60). The nail should be driven to a level
allowing the most inferior of the two proximal locking screws to be placed just
superior to the inferior (medial) cortex of the femoral neck. Proper rotation
of the nail also must be confirmed at this time. The 8° anteversion in the
proximal holes in the nail accommodates the normal anteversion of the neck, but
the proximal femoral fragment often sags, necessitating further external
rotation of the drill guide below the horizontal level to prevent proximal
screw placement posterior to the femoral neck. Oblique fluoroscopic C-arm views
can assist in ensuring accurate rotation of the drill guide.
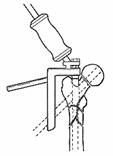
Fig.
27-60
Using
the multiple drill sleeves, a 3.2-mm threaded guide pin then is drilled through
the most distal of the proximal locking holes to a level about 5 mm from the
subchondral bone of the femoral head (Fig. 27-61). If anteroposterior and
oblique lateral views on the fluoroscope demonstrate errant position of the
guide pin, it is extracted and the nail is repositioned appropriately in the
femur. Anterior placement of the screws in the femoral head must be avoided.
The pin for the superior 6.4-mm screw then is placed similarly and its position
is confirmed on fluoroscopy (Fig. 27-62). Standard drills and taps are used
over the calibrated guide pin before screw insertion. Tapping is especially
indicated for dense bone in young patients. Routine distal targeting techniques
are used.
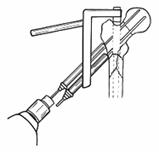
Fig.
27-61 Fig.
27-62
Depending
on the fracture pattern, quality of the bone, and purchase of the proximal
locking screws, protected weight bearing may be indicated after surgery.
Dynamization of the statically locked reconstruction nail usually is not
necessary.
Postoperative Care and Rehabilitation
After closed
femoral nailing, all patients should be mobilized out of bed as promptly as
feasible. Even the mere act of sitting up in bed or in a chair diminishes the
risk of pulmonary complications, especially in the patient with multiple
injuries. A major advantage of interlocking nails is that relatively pain-free
mobilization is possible even with highly comminuted fractures. Supplemental
external support in the form of traction or cast bracing rarely is necessary.
Dynamically locked nails with equivocal purchase on the unlocked fragment may
need protection against malrotation until the patient's muscle tone and
strength return. This is especially true for distal infraisthmal fractures that
can rotate externally on the nail. The use of a derotation boot in bed usually
suffices.
If
rigid fixation of the fracture is achieved, the patient can resume normal
muscle activity and joint motion as early as tolerated. Only mild analgesics
are required after the immediate postoperative period. Patients are instructed
in quadriceps-strengthening exercises and progressive weight bearing. Weight
bearing is delayed only in patients with very proximal or distal fractures that
are at risk for implant fatigue failure and in patients with ipsilateral
extremity injuries, such as knee ligament tears.
Prolonged
therapy under the guidance of a physical therapist usually is not necessary.
Full range of motion of the knee can be expected 4 to 6 weeks after a simple
nailing. Using dynamic quadriceps strength and isometric strength tests, Mira
and coworkers227 confirmed that the early and late range and strength of knee
motion are better after nailing than they are after either traction or cast
brace treatment.2
Serial
radiographs at 1, 3, 6, and 12 months after nailing should be obtained to
document fracture healing and remodeling. Dynamization of the statically locked
nail rarely is indicated except in cases of delayed healing at 3 to 4 months
after injury.59,60 When indicated, dynamization is accomplished by removal of
the screws farthest from the fracture because these screws contribute the least
to fracture stability.
Routine
nail removal is not mandatory.226 However, it is advisable in young patients 1
to 2 years after injury if fracture remodeling has proceeded normally. Earlier
extraction for relief of trochanteric pain from the proximal screw or proximal
tip of the nail is safe if the fracture is healed solidly.56 Distal screw heads
are a less frequent source of chronic discomfort. In the presence of delayed
fracture healing, removal of only the locking screws causing local symptoms
occasionally is indicated. Such screw extraction must be done judiciously to
prevent loss of fracture fixation.
Heterotopic
bone develops around the proximal tip of the nail in up to 20% of cases of
closed nailing.208,226,333 There is a positive correlation between bone
formation and certain patient and fracture variables, including the male
gender, the presence of a head injury, a high ISS, and a prolonged stay in the
intensive care unit (Fig. 27-63). A prominent tip of the nail above the
trochanter theoretically adds to the risk of heterotopic ossification, but
clinical studies have not confirmed its importance.208 The presence of an
ipsilateral acetabular or pelvic fracture can predispose to heterotopic
ossification, especially if an extensile approach through the gluteal muscles
is used for surgical fixation. Less than 5% of patients require reoperation
with nail extraction and ectopic bone excision for pain or restriction of hip
motion.
AUTHORS'
PREFERRED METHOD OF TREATMENT
Our 15-year
experience with closed interlocking nailing has convinced us that this
technique should be the treatment of choice for nearly all fractures of the
femoral shaft. More than 95% of the femoral fractures that we see at our
respective institutions-Parkland Memorial Hospital in Dallas and the Shock Trauma Center of the Maryland Institute for Emergency Medical Services System in Baltimore-are nailed. As a reflection of the high-energy nature of most femoral shaft
fractures treated at our trauma centers, locking screws are used in nearly all
these cases.
COMPLICATIONS
AND PITFALLS
The type and
severity of complications often are related to the specific treatment selected
for a given fracture. The prevalence of complications has dropped remarkably
with recent therapeutic advances, especially closed intramedullary nailing.87
Nerve Injury
The femoral and
sciatic nerves escape injury with most fractures of the femoral shaft. The
nerves are encased in muscles throughout the length of the thigh and are highly
resistant to stretch injuries during blunt trauma. The prevalence of nerve
injury is higher with penetrating trauma such as gunshot injuries.
Injuries
to the nerves during treatment of the shaft fracture can arise in several ways.
During skeletal traction on a balanced suspension splint, the leg tends to roll
into external rotation. If the proximal fibula rests on the splint, compression
palsy of the common peroneal nerve can occur, especially in heavily sedated
patients or patients with altered states of consciousness. This complication of
traction treatment can be prevented by adjusting the position of the leg on the
suspension frame, padding the area around the neck of the fibula, and
encouraging the patient to move freely in the traction system.
Intraoperative
nerve damage can result either from stretch injury due to excessive traction
for a difficult reduction or from direct compression due to poor positioning of
the patient on the fracture table. The pudendal and femoral nerves can be
compressed by an unpadded post of the table; careful padding of both the
horizontal and vertical posts protects these nerves.55,168 The likelihood of a
pudendal nerve palsy increases with the magnitude of the intraoperative
traction55 (Fig. 27-64). Either sensory or motor branches of the pudendal nerve
can be affected, but most palsies are transient. The sciatic nerve is injured
more frequently by stretch, especially when longitudinal traction is needed
during a delayed nailing. Traction with the hip flexed and the knee extended
increases the pull on the nerve and must be avoided.
Most
intraoperative nerve palsies can be prevented. Specific recommendations to
prevent the common pudendal palsy include completely relaxing the patient under
anesthesia, carefully positioning the patient on the fracture table, minimizing
the magnitude and duration of skeletal traction, and avoiding prolonged
adduction of the hip on the table post.55
Vascular Injury
Given the large
forces required to fracture a normal femoral shaft, it is surprising that major
vascular damage does not routinely accompany these fractures. Although the
perforating branches of the profundus femoris artery often rupture, resulting
in a tense fracture hematoma, damage of any nature to the superficial femoral
artery is documented in less than 2% of fractures.22,177 Because of its rarity
in civilian practice, vascular injury often is overlooked.
The
femoral vessel can be partially or completely torn, thrombosed, or merely
stretched and in spasm. Intimal tears can remain occult until the appearance of
late thrombosis.177,296 Although occlusion of a normal superficial femoral
artery does not inevitably result in irreversible gangrene because of abundant
collateral circulation through the profundus femoris artery, prompt diagnosis
and treatment of vascular injuries generally are imperative for preservation of
the limb (Fig. 27-65).
Fig.
27-65
Vascular
damage can accompany any fracture pattern but is most common with penetrating
trauma. The presence of diminished distal pulses should initiate a diagnostic
assessment of the vasculature of the limb. Although Doppler study of the distal
vessels may suffice, there should be no hesitation in ordering an arteriogram.
The indications for arteriography vary, but the study should be considered
seriously in limbs with absent pulses, all fractures secondary to penetrating
trauma, and distal fractures at the level of the adductor hiatus. Normal distal
pulses do not exclude a serious vascular injury, and repeated examination of
the limb is necessary to avoid missing an occult lesion.177
The
treatment of vascular injury should be a complementary team effort by vascular
and orthopaedic surgeons. The aim of surgery is to limit the period of ischemia
to the shortest possible time by prompt restoration of the arterial flow to the
limb. Irreversible muscle ischemia and extensive necrosis develop over a 6- to
8-hour period, depending on the extent of vascular occlusion and the adequacy
of intact collateral vessels. The vascular surgeons may restore circulation by
creating temporary shunts around both the arterial and venous injuries. Any
internal stabilization of the fracture then can be accomplished without a sense
of urgency. After fracture fixation, definitive vascular repair by direct
anastomosis or grafting can be performed. Such a staged repair is not necessary
if a simple, localized laceration to the artery can be repaired quickly.
Fasciotomies are indicated if there has been a delay in restoration of blood
flow or if compartment swelling is noted.
Multiple
factors must be assessed in deciding on the best management of the fracture.
The presence of open wounds, the degree of contamination, the location and
comminution of the fracture, the amount of soft-tissue necrosis, and the delay
before vascular repair all influence this decision. As a general rule, femoral
fractures associated with vascular injuries in civilian practice should be
stabilized internally, whereas those from war injuries should be treated on an
individual basis. The vascular surgery is simplified by open reduction and
internal fixation of the fracture.35
The
added risks of open fracture care are minimal in the closed, noncontaminated,
low-energy injuries seen in civilian fractures. War injuries are distinguished
by their contaminated wounds and frequent delays in treatment. During the
Vietnam War, 30% of acute major arterial injuries had an associated fracture.285
The high infection rate after open fracture fixation in this military
population has led to a preference for alternative modes of fracture
immobilization, including traction and external fixation. Connolly and
associates93 suggested that the arterial suture line is resistant to
longitudinal traction by both the elastic properties of the vessels and the
tether effect of the surrounding soft tissues. In their series of wartime
injuries, fracture instability in traction was not a source of failure of
vascular repairs. If extensive soft-tissue dissection is required for the
internal fixation of an open fracture, the risks of infection and resultant
failure of the vascular repair outweigh any benefits of internal fixation. The
decision regarding open versus closed treatment of the fracture should be made
jointly by the orthopaedic and vascular surgeons.
The
problem of late vascular compromise should be evaluated in all patients with
femoral shaft fractures. In a study of 30 patients who had suffered femoral
fractures 6 to 20 months before examination, an alarmingly high rate of occult
femoral artery injuries was discovered.22 A total of 15% exhibited hemodynamic
abnormalities using Doppler ankle-arm pressure indices, all in relation to
previously injured limbs. Although most of these subclinical vascular injuries
never adversely affect function, major late vascular complications, including
false aneurysm, arteriovenous fistula, and thrombosis of an intimal tear, have
been described.296
Most
limbs with vascular injuries can be salvaged by prompt repair of the vessels
and astute care of the fracture. The key determinants of limb survival include
the successful restoration of peripheral flow, the length of delay before
repair, the extent of disruption of the collateral circulation, the amount of
soft-tissue injury, and the presence or absence of infection.
Infection
Occasionally,
infection complicates intramedullary nailing of the femur. The prevalence of
infection is related to the technique of intramedullary nail
insertion,89,136,178 the use of supplemental fixation of the fracture site, and
the presence of open wounds (Fig. 27-66).
Before
the use of operative fluoroscopy, open intramedullary nailing was the standard
method of nail insertion.309 It required a moderate exposure and soft-tissue
stripping of the fracture site. Reports on the prevalence of infection after
the open technique have varied, with most large series documenting this
complication in 1.7% to 9% of cases.65,159,167,355 Some authors have contested
the observation that infection is more prevalent after open intramedullary
nailing as compared with closed nailing.139,187,309,363 The published data,
however, appear irrefutable. The series of Winquist and coworkers370 of more
than 500 cases of closed femoral nailing yielded a postoperative infection rate
of 0.9%. Investigations by King and Rush,175 Rothwell and Fitzpatrick,298 Esser
and colleagues,108 Wiss and coworkers,372 and Rothwell,297 each with more than
100 cases of closed intramedullary nailing, documented infection rates of 0.8%,
zero, 0.8%, zero, and zero, respectively. When the large series using these two
methods are compared, there is little doubt that open intramedullary nailing
carries a slight but significant increase in the risk of postoperative
infection.118
Comminuted
fractures managed by open nailing are especially at risk for postoperative
infection. The multiple fragments oblige the surgeon to use supplemental
fixation with cerclage wires. The combined stripping from the high-energy
injury and the surgical placement of the cerclage wires devitalizes the
cortical fragments. These devitalized fracture fragments serve as an excellent
nidus for infection.162,264,351 Interlocking nails, which obviate intrusion
into the fracture site for more stability, have largely replaced this
technique.
The
final factor that predisposes to postoperative infection after intramedullary
nailing is open wounds. When intramedullary nailing is applied to open
fractures of the femoral shaft, the prevalence of infection appears to be
related to the severity of the soft-tissue injury. Lhowe and Hansen,194
Winquist and colleagues,370 Chapman and Mahoney,77 and Brumback and
associates57 all have demonstrated that grade I, II, and III open fractures can
be nailed safely with a low risk of infection. Fractures with gross
contamination, exposed bone, and extensive soft-tissue necrosis (grade IIIB)
carry an unacceptably high risk of infection after nailing, regardless of the
treatment method.
Most
patients with infections have purulent drainage from a sinus in the thigh or
from the surgical incision in the buttock. Patients who have erythema,
swelling, or induration of the thigh weeks or months after intramedullary
nailing should be investigated for infection.158,179,201,366 Plain radiographs
should be scrutinized for periosteal reactive bone or a radiodense sequestrum
at the fracture site. Infected, necrotic cortical fragments can be obscured
easily by the radiopaque intramedullary nail. If a sinus is present, a sinogram
can be helpful in locating the nidus of the infection. The sinogram usually
reveals direct communication with the tip of the intramedullary nail at either
the insertion site or the fracture site. Tomography can assist in locating a
sequestrum. Computed tomography, ideally performed at the time of sinography,
can help in delineating communication of the sinus with different parts of the
femur. Unfortunately, computed tomography is subject to distortion from scatter
caused by the intramedullary nail. Blood analysis, including a white blood cell
count and sedimentation rate, should be obtained to determine the extent of the
patient's systemic response to the infection. A technetium or gallium
radionuclide scan may assist in diagnosing infection in the area of a healing
fracture, but the usefulness of this test in the presence of infection after
intramedullary nailing remains in question.266
Once
a deep infection is diagnosed, a decision regarding the advisability of nail
removal must be made. Most authors agree with the recommendations of MacAusland
and Eaton201 and Patzakis and coworkers,266 who advocate retention of the nail
if rigid fracture stabilization is provided by the implant. The fixation
provided by the nail is assessed best at the time of debridement of the
infection. If no gross motion is discernible in any plane, including rotation,
the nail should be left in situ. Because most femoral fractures heal within 4
to 6 months, even in the presence of infection, the patient must be protected
from septicemia during that time. Such protection is provided by thorough
debridement of all sequestra and infected soft tissue, care of the open wound,
and judicious use of antibiotics. Some authors have recommended wound closure
over suction-irrigation systems after debridement, but the threat of
superinfection has limited the popularity of this technique.266 If the
causative agent is sensitive to an oral antibiotic tolerated by the patient,
oral antibiotics can be used to suppress the infection during the time to
fracture union.266 After adequate fracture healing, the nail can be removed and
the endosteal canal should be reamed to remove the infected membrane and bone
from the canal. In severe infections, antibiotic-impregnated beads can be
placed down the canal after nail removal for further treatment of the
infection.
If
rigid fixation is not provided by the nail, several alternatives should be
considered. The degree of fracture stability can be augmented either by the
insertion of locking screws into an interlocking nail or by the use of a
larger-diameter exchange nail. If extensive sequestration of the femoral shaft
is present, removal of the nail, radical debridement of the femur, and
application of skeletal traction or an external fixator may be necessary (Fig.
27-67). Antibiotic-impregnated bead insertion into the segmental defect may be
advantageous. After a period of at least 6 weeks with the patient free from
wound drainage, staged reconstruction of the femur can be undertaken. This must
be individualized for each case and may require repeated intramedullary
nailing, bone grafting, or bone transport.
Delayed Union and Nonunion
In
contradistinction to diaphyseal fractures of the tibia, delays in healing of
femoral shaft fractures are rare. Delayed union implies a slow healing, longer
than what is reasonably expected for a given fracture. Any fracture of the
femoral shaft that is not healed by 6 months clearly qualifies as a delayed
union. Nonunion signifies a fracture that will not heal without some further
intervention. Numerical guidelines for defining delayed union and nonunion
remain arbitrary. Most cases of deficient bone healing arise from an
insufficient blood supply at the fracture site, uncontrolled repetitive
stresses, or infection. Specific factors that predispose to delayed union and
nonunion include open fractures, extensile operative stripping of the soft
tissues around the fracture site, inadequate fracture stabilization, fracture
distraction, infection, and (perhaps) a history of heavy smoking (Fig. 27-68).
Even in the presence of one or more of these factors, most femoral shaft
fractures heal rapidly after closed intramedullary nailing.
Once
the primary cause of slow healing is identified, the management of delayed
union usually is obvious. If dynamic intramedullary nailing has been used,
inadequate fracture stabilization may be the cause of delayed union or
nonunion. Whereas increased weight bearing may stimulate fracture union in
these cases, fractures demonstrating no evidence of callus response at 4 to 6
months after nailing are treated best with a reamed exchange nailing with a
larger-diameter nail. Fracture distraction after interlocking nailing can be
managed by dynamization of a statically locked nail, bone grafting around a
fracture gap, or reamed exchange nailing with a larger-diameter nail (Fig.
27-69). Slight shortening of the extremity is possible after dynamization, even
after 6 months of static interlocking. Although weight bearing with fracture
impaction after dynamization usually stimulates fracture union, leg-length
discrepancy can be accentuated in fractures already stabilized slightly shorter
than the noninjured contralateral extremity.60
Femoral
nonunion invariably requires surgical intervention to achieve union. Reamed
intramedullary nailing is ideally suited for most cases of nonunion of the
femoral shaft. In addition to providing a load-sharing, rigid stabilization of
the nonunion site, nailing and reaming stimulate neovascularization of the
shaft. A closed technique for reamed nailing is preferred whenever feasible.
Webb and associates357 reported a 95% union rate within 20 weeks in a series of
105 cases of femoral nonunion treated by intramedullary nailing. Nearly 80% of
the procedures were accomplished without exposing the nonunion site. Four cases
of nonunion that did not unite with intramedullary nailing subsequently healed
after exchange nailing with a larger nail. The open technique should be
reserved for cases of loose or broken plates, synovial pseudarthrosis, and
cases of displaced nonunion that cannot be reduced by closed means. Autogenous
bone grafting is advisable after excision and open nailing of a synovial
pseudarthrosis, but is unnecessary after nailing of most cases of hypertrophic
nonunion. When bone grafting is required, the reamings of the canal can be used
to supplement graft taken from the posterior iliac crest or the greater
trochanter.
One
study investigated the simultaneous correction of leg-length discrepancy in
association with therapy for nonunion of the femoral shaft. The technique
involves open debridement of the nonunion site with distraction by skeletal
traction. After bone grafting the defect, the wound is closed and static
interlocking nailing is performed. The authors reported union in 88% of the
patients and noted no neurovascular complications with an average lengthening
of 2.4 cm.381
Other
techniques, including femoral plating, electrical stimulation, and external
fixation with a rigid ring (Ilizarov technique) system, have limited
indications for the treatment of cases of femoral nonunion.
Malunion
There is no
consensus regarding what represents a malunion of the femoral shaft. An
anterior bow is compensated well by hip and knee motion and is tolerated better
than either a posterior bow or lateral angulation. Shortening up to 1 to 1.5 cm
is compatible with good function. Malunion commonly complicates shaft fractures
managed by traction or plaster immobilization. Because of the deforming
muscular forces, especially those of the adductors, most cases of malunion
after conservative treatment involve internal rotation, varus deformity, and
shortening of the femur. The rare malunion after internal fixation usually is
secondary to technical errors during the surgery, resulting in fixation of the
shaft in a malalignment. Postoperative external rotational deformity can follow
intramedullary fixation with small-diameter, unlocked nails.
External
rotational deformities after closed interlocking nailing generally are well
tolerated by patients. In an ultrasonic study measuring the torsional
deformities of 110 interlocked fractures, Braten and associates41 noted that 21
had external rotational malalignment of 15° or more compared with the opposite
normal femur. Only 8 patients expressed complaints related to the deformity and
only 3 required reoperation to correct it. The 26 patients with external
rotational malalignment of between 10° and 15° had few minor complaints. All
the deformities were attributed to incorrect positioning of the limb during the
nailing procedure. Careful attention to operative details should limit any
rotational malalignment to less than 15°.
Malunion
can result in an abnormal gait, a limb-length discrepancy, and post-traumatic
arthritis of the knee. The risks of knee arthritis from a malalignment of the
femur have been studied by Kettelkamp and associates.172 Fourteen patients were
evaluated using static biomechanical frontal plane analysis of the forces of
the knee. An increased force on the tibial plateau was strongly associated with
a varus or valgus deformity at the knee. The importance of restoration of lower
limb alignment also has been emphasized by many clinical investigators.
Most
cases of severe malunion are readily amenable to corrective osteotomy and
intramedullary nailing (Fig. 27-70). Because of translation or shortening at
the malunion site, open osteotomy and intramedullary nailing usually is
required. Closed osteotomy using a medullary saw under fluoroscopic control is
preferable for simple rotational malunion.
Refracture
Refracture
through a healed femoral fracture site is a rare event. It can occur, however,
at two times during the healing process: during early phases of callus
formation or at the time of hardware removal.
Fractures
treated by traction or cast bracing usually heal with abundant callus. Although
abundant in quantity, the trabeculae of new bone are not aligned along lines of
stress and are prone to fracture with major loading. More than 75% of the cases
of refracture reported by Seimon316 occurred within the first 3 to 4 weeks of
cast immobilization of the patient. Most were sustained during quadriceps
exercises, especially in those patients with limitation of knee motion.
Stiffness of the knee lengthens the lever arm acting on the fracture site and,
thus, increases loading and predisposes to refracture. After 8 to 12 weeks,
stress-induced remodeling of the callus lessens the chance of refracture.
Although
early refracture is negligible after operative fixation, refracture after
implant removal is still a serious problem, especially after plate fixation.
The biology of fracture healing after plate fixation differs from that after
nailing. Rigid plate fixation results in primary fracture healing, with
osteonal healing across the small cortical fracture gap. Callus should not be
evident on radiography. With primary fracture healing, the strength of the bone
at the fracture site is slow to return to normal, depending on the realignment
of the newly formed osteons by creeping substitution. Various theories,
including stress shielding, osteopenia of the bone beneath the plate, and slow
revascularization of the cortical bone, also have been offered to explain the
weakness of bone beneath a rigid plate. Premature removal of a plate (before a
minimum of 18 months from the time of application) can place the bone in
jeopardy of refracture. Breedenveld and coworkers44 noted a 13% refracture rate
in 148 shaft fractures, mostly after plate fixation. They advocated routine
cancellous bone grafting of all fractures with medial cortical defects.
The
generous callus envelope that develops after closed intramedullary nailing
protects the fracture site from refracture after nail removal. Refracture at a
different level has been an intraoperative problem during the extraction of
Zickel nails. The rigid, prebent design of the Zickel nail can cause transverse
fractures several centimeters below the lesser trochanter during nail removal.
The risk is high in young patients with normal cortical bone. In a series of 12
patients with refracture during Zickel nail extraction described by Ovadia and
Chess,255 all cases of refracture were different from the original fracture in
type and site. The authors recommended that the nail, in its current design,
not be used for subtrochanteric fractures in young patients.
Static
interlocking of the major fracture fragments to the intramedullary nail does
not appear to diminish the abundant callus that is seen with closed nailing or
to increase the likelihood of refracture.56,226 Theoretically, a statically
locked fracture may have a higher prevalence of refracture secondary to either
the stress riser effect of the locking screws or the stress-shielding
properties of the statically locked nail. However, bone density studies using
computed tomography have revealed that the stress-reducing effects of locked
intramedullary nails are small.40 In a series of 214 fractures treated with
statically locked nails, Brumback and colleagues56 noted only one case of
refracture. In 111 fractures in which the nail was left in situ, no subsequent
fractures occurred during 30 months of follow-up. The one case of refracture
that occurred in 103 femora from which the nail had been removed after fracture
union occurred through the site of the original fracture 6 weeks after removal
of the nail. None of the statically locked fractures had been converted to
dynamic nailing in either group. The authors concluded that the risk of
refracture after statically locked nailing is negligible.56
Implant Complications
In the past,
fatigue fracture of implants applied for fractures of the femur was common.
With advances in metallurgy and design, along with a fuller appreciation of the
major stresses to which any fixation device is subjected, the prevalence has
diminished.
Load-shielding
implants such as plates are prone to failure more often than are load-sharing
implants such as nails. In a series of 131 comminuted femoral shaft fractures
treated with ASIF plating techniques, Ruedi and Luscher300 reported 9 cases of
plate loosening or breakage. All 9 fractures had medial cortical defects that
increased the bending and tensile loading of the laterally placed plate. The
frequency of plate breakage and loosening can be reduced by avoiding fracture
distraction, routinely applying bone graft, delaying weight bearing, and using
broad dynamic compression plates. Because of the load shielding of the bone by
plates, however, breakage remains a problem. A plating that has failed by
either loosening or fatigue breakage is treated best by hardware removal and
intramedullary nailing.
Implant
failure after intramedullary nailing of a shaft fracture usually is associated
with either the insertion of a small-diameter nail or the use of an
interlocking nail for a very proximal or distal shaft fracture(see Biomechanics
of Intramedullary Nailing). Soto-Hall and McCloy329 noted that plastic
deformation (bending) of intramedullary nails occurs mainly with nails that are
10 mm or less in diameter (Fig. 27-71). Newer nails with closed-section designs
and thicker nail walls are less prone to plastic deformation and fatigue
failure. Nails can deform during surgery when they are inserted through a
tight, narrow canal, or after surgery with loading of the leg before fracture
union. Complete cracks in the midportion of nails are less common than is
plastic deformation (Fig. 27-72). An angulated nail can be managed either by
manipulation over the apex of the angle or by open transection of the nail. If
the nail is straightened successfully by manipulation alone, routine exchange
with a larger-diameter nail is prudent (see Fig. 27-43). A weakened nail can
become angulated again with minor loading. A bent nail that has not been
straightened successfully by manipulation should not be left in situ, because
its extraction after fracture healing may be impossible.